
探讨胎粪吸入综合征(MAS)的超声影像学特点及肺脏超声对MAS的诊断价值。
选取2014年8月至2015年10月根据病史、临床表现和胸部X线检查诊断为MAS的67患儿为研究对象,以100例无肺部病变的新生儿为对照,归纳和总结MAS的超声影像学特点。在安静状态下,患儿取仰卧、侧卧或俯卧位,以腋前线、腋后线为界,将每侧肺脏分成前、侧、后3个区域,探头与肋骨垂直或平行,分别对双侧肺脏的每个区域进行扫查。
本组MAS患儿的肺超声主要表现:(1)肺实变伴支气管充气征,见于所有患儿。通常重度患儿肺实变范围较大、边界不规则,轻度患儿则为局灶性小范围实变。(2)胸膜线异常和A-线消失,见于所有患儿。(3)肺不张,见于重度MAS患儿,本组12例(17.9%),严重大面积肺不张时还可见肺搏动。(4)胸腔积液,轻度或重度患儿均可见,本组9例(13.4%)。(5)所有患儿在非实变区呈肺间质综合征改变或表现为B-线。
MAS患儿具有典型的肺部超声影像学改变。由于准确、可靠、费用低、操作方便、无射线损伤,以及便于动态观察和及时了解病情变化,可常规用于MAS的诊断。

版权归中华医学会所有。
未经授权,不得转载、摘编本刊文章,不得使用本刊的版式设计。
除非特别声明,本刊刊出的所有文章不代表中华医学会和本刊编委会的观点。
胎粪吸入综合征(meconium aspiration syndrome,MAS)是因胎儿在宫内或产时吸入被胎粪污染的羊水而导致新生儿出生后以呼吸窘迫为主要临床表现的严重肺部疾病,多见于足月儿或过期产儿,其中10%~20%会发生气胸、5%~10%死亡,早期、正确诊断对指导治疗和改善预后有重要意义[1,2,3]。长期以来,MAS的诊断主要依赖典型的病史、临床表现和胸部X线检查等,而超声未被列入MAS的诊疗程序。近年来,本研究组已成功将肺脏超声用于呼吸窘迫综合征(RDS)、新生儿暂时性呼吸增快症(TTPN)、肺炎和肺不张等多种新生儿肺脏疾病的诊断与鉴别诊断[4,5,6,7,8],发现超声诊断新生儿肺脏疾病具有准确、可靠、可在床边开展、便于疾病的动态观察等优点,且无射线损伤,值得在新生儿病房内常规、广泛开展[9,10,11]。为进一步拓展肺脏超声在新生儿肺疾病诊断领域的应用,本研究试图探讨MAS的超声影像学特点和肺脏超声对MAS的诊断价值。
选择2014年8月至2015年10月在中国人民解放军陆军总医院附属八一儿童医院NICU住院,具有典型病史、临床表现和胸部X线检查并接受有创或无创机械通气治疗的67例MAS患儿为研究对象。胎龄35+4~42+4周(晚期早产儿5例);男39例,女28例;自然分娩41例、剖宫产分娩26例;出生体质量2 280~4 950 g。同期住院、无肺部疾病、并接受肺脏超声检查的100例新生儿为对照组。男59例,女41例;自然分娩57例、剖宫产分娩43例;出生体质量为2 550~4 780 g。2组患儿基本临床资料具有可比性,患儿家长均知情同意。本研究经过本院医学伦理委员会批准。
患儿均在入院后、机械通气治疗前或在机械通气治疗12 h内接受首次肺脏超声检查。使用仪器为Voluson E8、E10或Logiq e等型号超声诊断仪(美国GE公司生产),频率为10~14 MHz的线阵探头。在安静状态下,患儿取俯卧、侧卧或仰卧位,以腋前线、腋后线为界,将每侧肺脏分成前、侧、后3个区域,探头与肋骨垂直或平行,分别对双侧肺脏的每个区域进行扫查。
包括胸膜线、A-线、B-线与彗星尾征、致密B-线与白肺、肺间质综合征(AIS)、肺滑、肺实变、肺搏动、支气管充气征、动态支气管充气征、肺点、双肺点等[12]。
应用SPSS 16.0软件对数据进行统计分析,2组超声检查结果阳性率的比较采用Fisher′s确切概率法,P<0.05为差异有统计学意义。
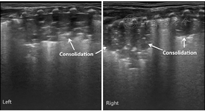
新生儿正常肺组织在超声下呈低回声,胸膜线与A-线均清晰显示,呈光滑、清晰、规则的高回声,二者与等间距平行排列;实时超声下肺滑清晰存在,无或可有少数几条B线;但无胸腔积液、肺实变(图1)。


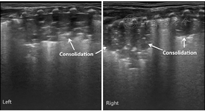
本组MAS患儿的肺脏超声主要表现(表1):(1)肺实变伴支气管充气征:见于所有患儿,重度患儿通常为范围较大、且边界不规则(锯齿状边缘)的实变区(图2,图3,图4);而轻度患儿则以小范围的局限性实变为主要表现(图5);但双侧肺脏实变范围的大小可以不同,而且同一侧肺脏野可以存在大小不同的实变区(图4,图5,图6)。(2)胸膜线异常与A-线消失,见于所有患儿,胸膜线异常表现为病变区胸膜线消失或增粗模糊(图2,图3,图4,图5,图6)。(3)肺不张,是严重肺实变的表现,见于重度患儿,本组12例(17.9%)(图7),严重大面积肺不张时可在实时超声下见到肺搏动和动态支气管充气征。(4)胸腔积液,见于9例(13.4%)患儿(图7)。(5)B-线或AIS,在实变区以外肺野则以AIS或B-线为主要表现。
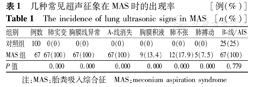
几种常见超声征象在MAS时的出现率[例(%)]
The incidence of lung ultrasonic signs in MAS[n(%)]
几种常见超声征象在MAS时的出现率[例(%)]
The incidence of lung ultrasonic signs in MAS[n(%)]
| 组别 | 例数 | 肺实变 | 胸膜线异常 | A-线消失 | 胸膜积液 | 肺不张 | 肺搏动 | B-线/AIS |
|---|---|---|---|---|---|---|---|---|
| 对照组 | 100 | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 25(25) |
| MAS组 | 67 | 67(100) | 67(100) | 67(100) | 9(13.4) | 12(17.9) | 5(7.5) | 67(100) |
| P值 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.779 |
注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome


注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome
注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome


注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome


注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome
注:MAS:胎粪吸入综合征 MAS:meconium aspiration syndrome
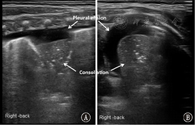
注:MAS:胎粪吸入综合征;A:探头与肋骨垂直扫描;B:探头与肋骨平行扫描 MAS:meconium aspiration syndrome;A:the probe was perpendicular to the ribs;B:the probe was parallel to the ribs
胎粪污染羊水(meconium staining of amniotic fluid,MSAF)的发生率为12%,但与胎龄有关,胎龄越大发生率越高,胎龄>42周者发生率可达30%以上,胎龄<37周者发生率低于2%,而胎龄在34周以下者则极少发生MSAF[13,14]。胎粪排出是胃肠道成熟的自然现象,在神经系统已经成熟的胎儿,脐带受压可引起短暂的副交感神经兴奋而引起胎粪排出,胎儿宫内窘迫也可诱发胎粪的排出。在胎儿出生开始自主呼吸后,可使胎粪颗粒吸至远端呼吸道。吸入大量黏稠胎粪者,患儿可于出生数小时内出现严重呼吸困难,表现为发绀、鼻翼扇动、三凹征和呼吸急促、呼气性呻吟等,严重者可致死胎或患儿出生后不久死亡。因此,早期明确诊断,对指导治疗、改善患儿预后意义重大。既往,MAS诊断主要依靠典型病史、临床表现、动脉血气分析和X线检查,但常导致误诊或延误诊断。
MAS具有典型的肺脏超声影像学改变。主要特征如下:(1)肺实变伴支气管充气征,见于所有患儿。通常重度患儿实变范围较大、边界不规则呈锯齿状,支气管充气征也较为明显;而轻度MAS则为较小范围的局灶型实变。(2)双侧肺脏或同一侧肺脏不同肺野病变性质与程度的不一致性,双侧肺脏可有范围不同的实变区,同一侧肺脏不同肺野也可以存在大小不同的实变区。(3)肺不张,见于少数重症患儿,更为严重者在实时超声下可见肺搏动或动态支气管充气征。(4)胸膜线异常,表现为病变区胸膜线消失或增粗、模糊。(5)A-线消失,所有患儿在实变区和非实变区均不见A-线。(6)B-线或AIS,非实变区肺组织在超声下常表现为B-线或AIS。(7)胸腔积液,轻度或重度MAS患儿均可有胸腔积液,本组见于13.4%的患儿。但上述超声表现也可见于RDS、肺不张和TTPN等肺病,虽均非MAS的特有改变,但均有各自的特点,超声很容易对它们做出诊断和鉴别诊断[4,5,6,7]。但在肺炎、尤其重度肺炎时,肺脏超声也表现为边界不规则的大面积肺实变[7,15],如无一定经验,仅靠超声表现有时难以将二者准确区别。因此,在借助超声诊断MAS与重症感染性肺炎时,往往需要结合病史。
总之,本研究对临床确诊为MAS的患儿进行了肺脏超声检查,并与无肺部疾病的新生儿对照比较,归纳和总结了MAS的肺部超声影像学特点,为MAS的超声诊断奠定了基础,是MAS诊断与鉴别的一种快速、简便、准确、无创的新技术。本研究的局限性在于研究对象均为病情较重(需接受有创或无创机械通气治疗)的患儿,病情较轻患儿的肺脏超声表现仍有待于进一步观察。作为一种新技术,开展肺脏超声尚需经过适当培训、操作者需要有一定的经验。



























