
外科治疗是炎症性肠病多学科治疗中的重要组成部分。本共识基于循证医学依据,采用Delphi方法制定,在克罗恩病(CD)、肛周CD和溃疡性结肠炎(UC)的外科治疗方面达成初步共识意见,以期为临床工作提供指导。

版权归中华医学会所有。
未经授权,不得转载、摘编本刊文章,不得使用本刊的版式设计。
除非特别声明,本刊刊出的所有文章不代表中华医学会和本刊编委会的观点。
炎症性肠病(inflammatory bowel disease,IBD)主要包括克罗恩病(Crohn′s disease,CD)和溃疡性结肠炎(ulcerative colitis,UC)。近年来IBD在我国的发病率逐渐增加,迫切需要适合我国国情的IBD诊疗方案。目前IBD的治疗主要包括内科治疗和外科治疗,内科治疗进展并未从根本上解决并发症和药物治疗无效的问题,因此外科治疗具有重要意义。
本共识采用Delphi程序制定,首先由中华医学会消化病学分会炎症性肠病学组外科俱乐部组织部分IBD外科专家,按照CD、肛周CD、UC 3个部分分别对国内外相关文献进行检索、筛选、整理、评价,确定共识意见需阐明的问题及推荐方案,参考国外共识并根据国内多位IBD外科专家的临床经验完成初稿;然后广泛征求国内IBD权威专家学者对初稿的意见并进行修改完善,形成初步共识意见;最后由《中华炎性肠病杂志》组织IBD领域专家对共识逐条讨论修改,进行投票并由第三方计票。投票等级分为a完全赞成(必不可少);b部分赞成,但有一定保留;c赞成,但有较大保留;d不赞成,但有一定保留;e完全不赞成。本共识意见中的推荐等级根据投票结果分为A级指标(强烈推荐),即a得票数为80%及以上;B级指标(推荐),即a和b得票数相加为80%及以上;C级指标(建议),即a、b和c得票数相加为80%及以上;未达C级指标则删去。最终由专家审阅定稿形成本共识意见。根据证据级别高低及专家投票结果,本共识将推荐等级分为"强烈推荐"、"推荐"和"建议"3个等级。
1.对CD肠狭窄导致反复或慢性肠梗阻者推荐手术治疗,炎性狭窄和无症状的肠狭窄可暂不手术。推荐等级:推荐
对于无临床症状的肠狭窄和炎性狭窄,诱导和维持疾病缓解是主要治疗目标。以纤维性狭窄为主或药物治疗无效的狭窄,可导致反复腹胀、腹痛,伴狭窄近端肠管明显扩张,影响患者进食,恶化营养状况,降低生活质量,推荐择期手术治疗[1,2]。
2.对局限性穿透型CD反复发作或无法排除癌变者推荐手术治疗。推荐等级:强烈推荐
穿透型CD可形成肠壁深大溃疡,溃疡的存在不但增加机体炎症负荷,增加药物诱导、维持缓解的难度,还常造成肠内瘘、肠外瘘或反复消化道出血,甚至癌变[2]。对于药物治疗效果不佳、病变局限但长期不愈合的CD深大溃疡,推荐手术切除[2];对于CD肠内瘘和肠外瘘患者,即使保守治疗后肠瘘暂时闭合,短期内避免手术,但由于存在肠壁溃疡,肠瘘容易复发,最终多数患者需要手术治疗[3,4];诊断明确的CD癌变强烈推荐手术,对于诊断困难、不排除癌变但无法获取病理学证据的慢性病灶,推荐手术切除[5]。
3.CD急性肠穿孔伴弥漫性腹膜炎时,推荐行急诊手术。推荐等级:强烈推荐
CD肠穿孔伴弥漫性腹膜炎强烈推荐急诊手术,术中除了清除腹腔污染外,还要切除穿孔肠段或部分组织送病理检查。考虑到腹腔污染对肠吻合的不利影响,急诊手术过程中推荐实施肠造口术[6]。如果肠穿孔面积较小,腹腔污染轻,可以在密切监测下先尝试保守治疗,争取非手术或择期手术。十二指肠穿孔不宜造口,可以行瘘口修补,并行胃十二指肠置管减压,保证修补口以下部位的肠管通畅,以便术后给予肠内营养(enteral nutrition,EN)。
4.CD伴消化道大出血若保守治疗无效时推荐手术治疗。推荐等级:强烈推荐
CD伴急性消化道大出血发生率为0.9% ~ 6.0%,其发病急,病情重,非手术治疗困难,病死率较高[2]。这类患者多有CD反复发作史,诊断较明确,出血部位多在病变最严重处,但仍需要排除其他疾病如胃肠道血管畸形、Meckel憩室炎等引起的出血。准确判定出血部位对治疗具有决定性意义。数字减影血管造影(DSA)结合CT等影像学检查有助于病因诊断和出血部位的判断。由于肠系膜血管结构的特殊性,介入栓塞治疗容易造成肠缺血甚至坏死,不宜作为确定性治疗手段[7]。对危及生命的大出血、非手术治疗失败者,强烈推荐急诊手术切除病灶以控制出血[8]。
5.对药物及营养治疗效果不佳、影响生长发育的儿童和青少年CD患者推荐手术治疗。推荐等级:推荐
儿童和青少年CD占CD患者总数的25%,其中大部分发生于青春前期或青春期,10% ~ 40%的CD患儿出现生长发育迟滞[9],慢性活动性炎症和营养不良是影响CD患儿生长发育的主要因素[10]。如果药物治疗、营养治疗无法有效控制疾病活动且病灶局限者推荐手术切除,可使病情进入缓解期,再积极地给予营养治疗和药物治疗,保证儿童和青少年正常生长发育[11]。对于青少年难治性广泛结肠CD,结肠切除促进生长发育的效果优于转流性回肠造口[11,12],但需要重视肠造口对患儿心理状况的影响。青春后期进行结肠切除对身高增长是否有促进作用尚不清楚[13]。
6.择期手术前推荐进行手术并发症风险评估。推荐等级:推荐
择期手术前强烈推荐由IBD专业的多学科团队(MDT)对患者进行手术并发症风险评估,并进行有针对性的预康复(prehabilitation)。目前尚缺乏公认的针对CD的术前评估体系,评估内容主要包括患者一般状况、营养状况、既往史与合并症、吸烟情况、血红蛋白水平、炎症程度及并发症等。评估手段包括营养风险筛查和营养状况评估、血清学、影像及内镜检查等。腹腔内环境及手术难度对手术成败有较大影响,评估时应予以重视[14,15]。
7.营养不良、合并感染、使用糖皮质激素、疾病活动以及腹腔解剖结构复杂是CD手术并发症的风险因素。推荐等级:强烈推荐
患者病情严重程度与手术后感染性并发症的发生风险有关[16],营养不良或具有营养风险(过去3个月内体质量减轻>5%)、低白蛋白血症(白蛋白<30.0 g/L)、贫血(血红蛋白<100 g/L)、使用糖皮质激素(以下简称"激素")[17,18]、合并腹盆腔感染以及穿透性病变是手术并发症的独立风险因素[19]。手术野局部条件如腹腔粘连、肠瘘等造成的解剖结构异常会延长手术时间,增加手术并发症的发生风险[20]。
8.对存在手术并发症风险因素的择期手术患者推荐进行术前预康复。推荐等级:强烈推荐
对于存在手术并发症风险因素的择期手术患者,强烈推荐进行有针对性的预康复[21],也称术前优化(preoperative optimization),以消除手术并发症风险因素,减少手术并发症[22]。具体措施包括纠正营养不良、诱导活动期疾病缓解、尽量撤减激素、通过引流和使用抗生素等措施控制腹腔或腹膜外感染等。
9.对存在营养风险、合并营养不良及处于疾病活动期的患者推荐实施术前营养治疗。推荐等级:强烈推荐
营养治疗,尤其是全肠内营养(exclusive enteral nutrition,EEN)具有纠正营养不良和诱导CD缓解的双重作用。EEN通过改善患者营养状况,替代激素及生物制剂诱导CD缓解,发挥从药物治疗转向手术治疗的桥接作用,提高CD手术的安全性。无法实施EN者建议给予全肠外营养(total parenteral nutrition,TPN)[23]。
10.对于合并腹腔脓肿的患者,推荐依据脓肿特点进行有效的引流。推荐等级:强烈推荐
强烈推荐在确定性手术前消除脓肿及蜂窝织炎等腹腔感染性并发症,具体措施包括抗生素、经皮脓肿穿刺引流和手术引流[24]。小脓肿(<3 cm)及不宜穿刺引流的蜂窝织炎推荐使用抗生素治疗[25],部分蜂窝织炎在感染局限为脓肿后可行穿刺引流[26];≥3 cm的腹腔脓肿首选经皮穿刺引流[27],采用CT或超声引导、选用较大口径的引流管和主动引流的方式能够提高引流效果[28];经皮穿刺引流效果不佳或引流失败、无法进行穿刺引流(毗邻大血管、肠袢间脓肿或没有合适的穿刺路径)时推荐行手术引流[27,28,29]。纠正营养不良有助于控制感染,营养治疗首选肠内途径,但使用过程中要注意观察患者反应,避免使感染恶化[28]。
11.术前尽可能停用激素。推荐等级:推荐
术前使用泼尼松>20 mg/d或相当剂量的其他激素>6周可增加术后感染性并发症的风险,激素联合使用其他免疫调节剂患者术后发生感染风险更高[30]。推荐术前停用激素,但停用时间尚无一致意见,一般认为用量越大,使用时间越长,停用需要的时间越长。长时间、大剂量使用激素者,停用过程中及术中、术后要警惕肾上腺皮质功能不全。对疑似肾上腺皮质功能不全患者建议临时补充适量激素,必要时检测肾上腺皮质功能[31]。对于病情较重、没有机会完全撤除激素就必须手术的患者,建议遵循损伤控制外科(damage control surgery)理念指导手术方案[32],并警惕发生肾上腺皮质功能不全。
12.巯嘌呤类药物在围手术期可以安全使用,抗肿瘤坏死因子-α单克隆抗体对术后并发症的影响尚不明确。推荐等级:推荐
术前使用硫唑嘌呤或6-巯基嘌呤不会增加术后并发症,术前使用抗肿瘤坏死因子-α单克隆抗体(以下简称"抗TNF-α单抗")与术后并发症的关系尚存争议[33,34],检测抗TNF-α单抗血药浓度对术后并发症的指导价值暂无定论[35,36]。因此,对近期使用过生物制剂的择期手术患者,充分的预康复更为安全;对于迫切需要手术的患者,不能因为没有停用生物制剂或者停用时间不足而推迟手术,但应重视预康复;对于存在术后并发症风险因素的患者,注意预防术后并发症[35,36,37]。
13.对完成预康复的患者重新进行病情评估,以决定后续治疗方案。推荐等级:强烈推荐
多数患者通过预康复可达临床缓解[38,39]。建议在预康复完成后重新进行生化指标、影像学等全面评估,是否进行确定性手术取决于药物治疗能否维持疾病长期缓解,恢复患者正常生活质量。如果需要手术或内镜治疗,预康复完成后是最好时机,应及时安排[40];如果预计恢复进食后症状不会复发,则根据复发风险选择适当的药物维持缓解[28]。
14.预康复效果不明显或者失败时,推荐采取损伤控制手术缓解症状。推荐等级:强烈推荐
在预康复过程中建议进行动态评估,如果患者病情无好转甚至恶化或患者的生理储备和脏器功能状态欠佳,应权衡继续进行预康复与尽快手术之间的利弊,调整治疗方案[22]。如果选择手术治疗,应遵循损伤控制外科理念制定手术方案[41]。
15.外科医生要做好充分的术前准备。推荐等级:强烈推荐
手术组医生的准备包括充分了解病情、制定手术预案、准备手术器械和药品以及安排手术人员等。术前需系统回顾患者病情和仔细体检,认真阅读小肠CT造影(CTE)或磁共振小肠造影(MRE)、消化道造影等影像图片[42],明确病灶部位、累及范围和严重程度、肠瘘来源、是否合并脓腔等解剖学改变以及手术野粘连程度等情况[43],上述信息对制定治疗方案极为重要[44]。
16.重视手术患者的心理准备。推荐等级:强烈推荐
患者的术前准备包括生理和心理准备[45],预康复主要完成生理准备。患者对手术的知晓程度(包括手术目的、方式和结果、术后可能出现的并发症及处理方案等)、患者的家庭状况、亲属的态度都会对患者心理状态产生巨大影响,并最终影响手术决策和治疗效果,因此,需要重视患者术前的心理准备。推荐通过术前宣教、患者相互交流、互联网和多媒体等现代技术手段,将手术方案、目的、手术预期、术后治疗与医疗团队的联系方式等内容向患者及其亲属进行详细说明,结合患者的需求制定个体化的治疗方案,以取得其理解、信赖与配合。
17.推荐采用加速康复外科理念促进术后患者康复。推荐等级:推荐
推荐在CD外科治疗过程中遵循加速康复外科理念(enhanced recovery after surgery,ERAS),通过减少应激、微创手术、术后镇痛、早期给予EN等措施促进肠功能恢复和体力恢复,降低术后并发症发生率及再入院率,缩短术后住院时间,减少医疗费用[46,47]。
18.狭窄型十二指肠CD行内镜球囊扩张术效果不佳时,推荐狭窄成形术。推荐等级:推荐
50% ~ 60%的十二指肠CD位于胃远端或十二指肠球部,25% ~ 30%位于降部和水平部,10% ~ 15%位于水平部和升部。十二指肠CD狭窄型多见,表现为幽门或十二指肠梗阻,10%的患者表现为多处狭窄[48,49]。
内镜球囊扩张术(endoscopic balloon dilation,EBD)是治疗十二指肠狭窄的首选方式,其方法简便,短期效果满意,但大多数患者需要反复扩张[50]。十二指肠狭窄成形术具有操作简单、安全、症状改善迅速、疗效确切、术后再发率低的特点,常用于治疗十二指肠球部、降部和水平部的单发狭窄[51]。狭窄靠近胃窦时可行胃大部切除术,但如果十二指肠球部炎症明显,与残胃吻合或关闭十二指肠时会有难度。术后建议服用质子泵抑制剂,不建议行迷走神经切断术[52]。
19.穿透型CD累及胃或十二指肠形成内瘘时,推荐切除原发病灶,对受累及的胃或十二指肠瘘口进行修补。推荐等级:推荐
胃或十二指肠穿透型病变多为邻近器官侵袭所致,比如回结肠、横结肠CD或回结肠吻合口CD再发累及胃或十二指肠,造成内瘘。穿透型CD累及胃或十二指肠的治疗原则是切除原发病灶,对受累的胃或十二指肠瘘口进行缝合修补[53]。该术式疗效满意,术后并发症发生率低,远期效果可靠[54,55]。但与结肠CD累及十二指肠相比,回结肠吻合口-十二指肠内瘘患者术后住院时间长、再次出现内瘘的可能性大[56]。理论上讲,右半结肠切除时回结肠吻合口应尽可能置于远离十二指肠的位置并用大网膜包裹,但有时因解剖限制,临床不易实施。
20.推荐术中完整探查全部小肠,详细描述切除及残存病变特征,准确测量并记录保留的小肠长度。推荐等级:强烈推荐
CD手术前通过影像学手段检查食管、胃、十二指肠和结直肠比术中探查方便准确,但对小肠的检查却不如术中探查方便。因此,虽然术前必须对小肠进行影像和内镜评估,术中仍然要完整、仔细地探查全部小肠,详细记录病变数量、每处病变的性质(炎症、狭窄或穿透)、严重程度、长度及相互距离,根据探查结果确定手术方案,并为术后治疗甚至再手术保留依据。术中探查容易遗漏短段狭窄型病变,并导致术后肠梗阻甚至短时间内再手术[57,58],应引起临床重视。
21.CD手术不但要缓解肠道症状,更要尽可能保留小肠。推荐等级:强烈推荐
对于局限性小肠病变,手术切除病变小肠能够有效缓解胃肠道症状,但对于多节段小肠病变,应遵循节约肠管的原则,不建议行大面积肠切除手术。预计切除范围>100 cm、确诊的短肠综合征或存在短肠风险、术后1年内再发可能性大的肠狭窄推荐采用狭窄成形术[59]。对多处小肠狭窄者可以进行多处狭窄成形术,或者切除最主要病灶,对其他部位行狭窄成形术。可供选择的术式有Heineke-Mikulicz、Finney及Michelassi等狭窄成形术[60,61]。对内镜可及的短段型(<4 cm)且不合并瘘、蜂窝织炎、活动性炎症的胃肠道纤维狭窄以及回结肠吻合口狭窄,推荐采用EBD治疗[1,62]。在实施狭窄成形术或EBD治疗之前,必须确定狭窄肠段无癌变。
与狭窄型病灶不同,药物治疗无效的穿透性病灶不但破坏病变肠段,并且会累及周围组织器官,因此推荐切除。但受累器官本身可能并非CD原发灶,甚至不是胃肠组织(如膀胱、阴道等),不具备CD发病基础,可以修剪后直接修补或行局部切除[4,63]。
22.术中意外发现的肠道CD如果没有手术指征,不建议切除。推荐等级:推荐
部分患者因其他原因(比如阑尾炎)手术,术中探查意外发现肠道CD。如果CD病灶有手术指征,并且术者是专业的IBD医生,建议手术处理;对手术指征不强的病灶,考虑到CD术后发生并发症的风险,建议留待术后全面评估和正规药物治疗;诊断明确的阑尾炎建议切除阑尾,但CD患者阑尾切除术后腹腔脓肿和肠瘘的风险明显升高[64]。
23.结肠狭窄首选切除,不建议行狭窄成形术。推荐等级:强烈推荐
结肠CD狭窄发生率高达17%,即使无症状结肠狭窄也有约7%的隐匿性癌变。由于存在闭袢性肠梗阻的风险并妨碍结肠镜下对近端结肠的观察活检,因此结肠狭窄首选手术切除,不建议行狭窄成形术。EBD和自膨式支架植入不宜作为确定性治疗手段,仅可用于暂时缓解肠梗阻症状,以便进行预康复,为确定性手术创造条件[65]。
24.对药物治疗失败的广泛结肠CD,推荐行全结肠甚至结直肠切除。推荐等级:推荐
对于药物治疗失败、并发结肠梗阻、重症结肠炎或严重肛周感染的结肠CD,转流性肠造口虽然能够暂时缓解临床症状,但不能逆转结肠病理改变,甚至进展为肠道泌尿系统内瘘或诱发癌变,生物制剂治疗也不能改善最终结局[66,67]。因此,对于反复发作、严重影响生活质量的广泛结肠CD,或可疑癌变甚至已经发生癌变者,推荐切除结肠。为避免出现性功能、生育及排尿功能异常,对于年轻、有生育意愿的患者可以暂时保留直肠,但应积极治疗,密切随访[68]。如需切除残余直肠,推荐经肛经腹联合括约肌间切除术式。
25.对于结肠CD,建议谨慎实施回肠储袋肛管吻合术。推荐等级:强烈推荐
对于结肠CD,结肠切除并回肠造口的性价比更高[69],回肠储袋肛管吻合(ileal pouch anal anastomosis,IPAA)术后并发症多,储袋失败率高达30%,仅限于肛周和小肠无病变、直肠肛门功能完好、且患者保肛意愿强烈、愿意承担后期储袋失败甚至切除的风险并能坚持药物治疗的CD患者[70]。结肠CD的IPAA手术建议采用J型储袋、双吻合技术,不建议采用黏膜剥除术。术后如发生严重盆腔感染或储袋相关并发症时,建议采用回肠转流性造口或者储袋切除术,不建议行挽救性储袋重建手术[71]。
26.行中上段小肠造口的同时推荐建立肠液回输途径,以应对术后肠液高排量。推荐等级:强烈推荐
小肠造口术后肠液高排量造成的脱水和急性肾功能不全较常见,是造口术后再入院的主要原因之一。对中上段小肠造口的患者,强烈推荐行远端小肠插管或外置造口,术后将近端肠造口排出的消化液连同EN经远端造口及时回输[72]。这项措施除了能够维持内稳态和营养需求外,还能保持远端肠管的生理功能,避免转流性肠炎,减少造口还纳术后肠麻痹等并发症风险[73]。造口期间需准确测量每天的肠液丢失量和尿量,以便及时纠正脱水,避免急性肾损伤。
27.对初次手术的回结肠或结直肠CD者推荐行腹腔镜手术,对复杂CD推荐行开放手术。推荐等级:推荐
对于有经验的外科医生,采用腹腔镜技术行结直肠CD手术能够促进患者术后恢复,降低手术部位感染等近期和远期并发症发生率和病死率[74]。腹腔镜手术治疗小肠CD的优势并不明显,单孔腹腔镜技术不优于多孔腹腔镜[75]。对于复杂内瘘、严重腹腔粘连、肠系膜炎性增厚及十二指肠CD,由于解剖结构复杂、探查容易遗漏病灶、腹腔容易污染、操作困难耗时等不利因素,推荐行开放手术[76]。对于危重症患者,由于腹腔镜手术耗时较长,有急性炎症的肠组织及其系膜处理较困难,建议行开放手术。
28.推荐CD手术使用直线切割吻合器行侧侧肠吻合。推荐等级:推荐
器械吻合较手工缝合术后住院时间短,吻合口漏和临床再发的概率低[77]。吻合方式并不影响CD术后内镜再发,但可能影响远期再手术率[78]。由于肠管直径、血供等原因的影响,侧侧吻合术后吻合口漏的发生率低于端端吻合术,是更合适的吻合方式[79]。侧侧吻合口并非越大越好,过大的侧侧吻合口可形成盲袋,由于难以排空和细菌过度繁殖,容易引起腹胀不适[80]。
29.推荐CD手术采用可吸收线缝合肠管,避免使用丝线。推荐等级:强烈推荐
可吸收缝线有足够的张力强度,组织反应轻,在体内经水解吸收,不引起线结残留、异物肉芽肿及缝线相关感染,单股线还能防止细菌附着,减轻组织切割、吻合口水肿、溃疡和出血[81]。丝线的成分是异种蛋白,会诱发吻合口慢性炎症反应。研究证实,与不可吸收丝线相比,可吸收线能够减少术后临床和内镜再发[82]。
30.CD术后发生吻合口漏或腹腔脓肿时推荐主动行肠造口术。推荐等级:推荐
CD患者术后感染性并发症发生率高于其他手术患者[83],治疗的核心是早发现、早处理,拖延处理会导致病死率增加,CD复发时间显著前移[84]。对可疑腹腔感染者要积极进行血清学和影像学检查,充分引流腹腔积液,引流效果不佳或考虑吻合口漏时,要果断进行转流性造口[85]。
31.术后早期肠梗阻首选非手术治疗。推荐等级:强烈推荐
肠麻痹与梗阻是IBD术后早期常见并发症,可以通过纠正内稳态和营养治疗,必要时给予激素促进缓解;梗阻症状明显时建议放置小肠减压管,不但能够进行肠腔减压,而且通过注射水溶性造影剂能够明确梗阻性质,促进梗阻缓解[86];合并腹腔积液或脓肿时建议充分引流;个别患者可发生机械性肠梗阻或者内疝,应注意鉴别,对非手术治疗失败者及时进行手术处理[86]。手术前后口服肠动力药有助于术后胃肠功能的恢复[87]。
32.术后肠吻合口出血首选非手术治疗。推荐等级:推荐
CD术后早期肠吻合口渗血较多见,可采用非手术治疗的方法进行控制。严重出血发生率约3%,与吻合方式、肠壁厚度、吻合器成钉高度、吻合口与肠管系膜缘的距离等因素有关,侧侧吻合口如果距离系膜缘太近,容易出现吻合口出血[88]。吻合完成后建议直视下检查,对活跃出血或可疑出血点采用缝扎止血。术后吻合口出血首选非手术治疗,无效者建议行DSA检查和内镜止血[89],对于出血量大、生命体征不稳者应及时进行手术处理。
33.推荐常规进行静脉血栓栓塞症风险评估,中高风险者采用预防性抗凝治疗。推荐等级:强烈推荐
IBD患者术后发生静脉血栓栓塞症(venous thromboembolism,VTE)的风险较高,使用激素、疾病活动、手术及卧床等原因均会增加VTE的风险,推荐根据共识意见采取积极措施进行防治[90]。早期下床活动是预防VTE最简单有效的措施,也符合ERAS路径。对于高度疑诊VTE的患者,如果没有绝对药物禁忌,建议先给予药物治疗,在VTE确诊后再考虑是否选择溶栓、下腔静脉滤器植入等介入治疗[91]。
1.有症状的复杂性瘘管型肛周CD、直肠阴道瘘、肛周脓肿、肛管直肠狭窄以及无症状但不能行结肠镜检查的肛管直肠狭窄推荐手术治疗。推荐等级:推荐
对于有症状的复杂性瘘管型肛周CD、直肠阴道瘘、肛周脓肿和肛管直肠狭窄推荐手术治疗。对于合并不可控制的脓毒症、难治性肛周CD或肛门失禁患者,推荐行转流性肠造口或直肠切除术[96]。无症状的肛管直肠非炎性狭窄若不能行结肠镜检查,影响对肠道的监测,推荐手术处理。肛周CD局部癌变者应及时进行包括手术在内的综合治疗。
2.无症状的肛周CD不建议手术。推荐等级:推荐
美国胃肠病学会(American Gastroenterological Association,AGA)将肛瘘分为简单性肛瘘和复杂性肛瘘两类[97]。无症状的肛周CD不建议手术[98]。对于药物治疗有效的无症状肛周脓肿(<1 cm),也不建议手术[99]。无症状的肛管直肠炎性狭窄、肛裂、疣状皮赘、痔、溃疡等建议采取非手术治疗[100]。
3.麻醉下探查联合盆腔MRI或腔内超声是肛周CD术前检查的金标准。推荐等级:强烈推荐
MRI具有无创、无辐射、快速、准确的优势,可精确评估瘘管或肛周脓肿的解剖结构和肛管直肠狭窄的范围及性质。根据盆腔MRI可对肛周疾病活动度进行准确的评价[101],也可与骶前囊肿、直肠间质瘤、骶尾部藏毛窦、肛周软组织肿瘤等其他肛周疾病进行鉴别,是肛周CD诊断及分型的首选方法[102]。麻醉下肛门探查联合盆腔MRI或腔内超声可使肛周CD诊断准确率达到100%[103]。
4.肛周症状评估及体格检查是评价瘘管型肛周CD活动度和疗效的主要手段,影像学检查也是重要手段。推荐等级:推荐
肛周疾病活动指数(perianal disease activity index,PDAI)对肛周症状和肛周体格检查进行量化评估,是评价瘘管型肛周克罗恩病活动度和疗效最常用的指标,准确率高达87%[104]。该评分包括肛周分泌物、疼痛与活动受限情况、性生活、肛周表现和硬结5个方面,单项评分按严重程度分为0 ~ 4分,总分最高为20分,PDAI>4分提示存在活动性瘘管或局限性炎症。建议采用表1所示方法对瘘管型肛周CD的疗效进行描述[99]。影像学检查是肛周CD的重要检查手段,基于影像学的3D重建可以更好地了解瘘管的走行方向[105]。
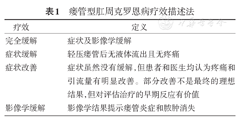
瘘管型肛周克罗恩病疗效描述法
瘘管型肛周克罗恩病疗效描述法
| 疗效 | 定义 |
|---|---|
| 完全缓解 | 症状及影像学缓解 |
| 症状缓解 | 轻压瘘管后无液体流出且无疼痛 |
| 症状改善 | 症状虽然没有缓解,但患者和医生均认为疼痛和引流量有明显改善。部分改善不是最终的理想结果,但对评估治疗的早期反应有价值 |
| 影像学缓解 | 影像学结果提示瘘管炎症和脓肿消失 |
5.有感染症状的肛周脓肿或瘘管型肛周CD强烈推荐行急诊挂线或置管引流。推荐等级:强烈推荐
挂线或置管引流可以充分引流瘘管和脓肿,控制肛周感染,减少脓肿、瘘管再形成的机会[106],是有感染症状的肛周脓肿或瘘管型肛周CD早期处理的首选方式[107]。表浅的脓肿或瘘管建议挂线引流,较大或复杂脓腔建议手术切开结合置管引流。挂线引流也可以用于瘘管的维持治疗和使用生物制剂及其他免疫调节剂期间感染的预防[108]。在挂线引流基础上使用生物制剂治疗瘘管型肛周CD的疗效优于单独使用生物制剂[109]。
6.肛管直肠炎性狭窄推荐药物治疗,纤维性狭窄首选机械扩张。推荐等级:推荐
对于伴有活动性结直肠炎和肛管狭窄的肛周CD患者,为避免损伤肛门括约肌,不建议手术治疗,可给予生物制剂、抗生素、免疫调节剂等治疗以促进炎症消退,缓解症状[110]。手指、球囊和器械扩肛适用于以纤维化为主的有症状的线状肛管直肠狭窄。对机械扩张治疗无效的线状肛管直肠纤维性狭窄(狭窄长度<4 cm)可行内镜下狭窄切开术或经肛狭窄松解术[111]。
7.推荐在疾病缓解期、不合并感染时进行肛周CD的确定性手术。推荐等级:强烈推荐
确定性手术治疗能缓解肛周CD临床症状,治愈瘘管和狭窄。手术成功率与肠道炎症、感染控制程度、营养状况和激素使用情况等密切相关。在控制活动性炎症和感染的前提下进行手术可减少确定性手术失败率和反复手术的风险[112]。当满足以下条件时,可实施确定性手术:(1)CD活动度评分(CDAI评分)正常;(2)内镜检查溃疡愈合;(3)肛瘘外口无明显分泌物,无新发脓肿或瘘管;(4)挂线和药物治疗前后MRI显示炎性病灶明显缩小,无新发或复发脓肿形成[100]。
8.在保护肛门功能的前提下选择肛瘘确定性手术方式。推荐等级:强烈推荐
瘘管型肛周CD确定性手术方式有瘘管切开术、经括约肌间瘘管结扎术(LIFT手术)、直肠推移瓣修补术、切割性挂线术以及肛瘘栓等,上述术式应在充分保护肛门功能的前提下选择使用。肛瘘切开术用于治疗低位单纯性肛瘘(瘘管通过肛门外括约肌的下1/3)的治愈率为80% ~ 100%[113],但因存在肛门失禁的风险,应避免用于女性前侧方肛瘘的治疗[114]。LIFT手术可用于治疗复杂高位肛瘘,治愈率为67%[115,116]。直肠推移瓣修补术也适用于复杂高位肛瘘和直肠阴道瘘,其治愈率报告不一,波动在25% ~ 64%,肛门失禁率约10%[117,118];如果初次手术失败,可尝试再次修补,但多次手术会增加肛门失禁的风险;在抗TNF-α单抗治疗期间进行修补可提高瘘管型肛周CD的长期愈合率[119]。切割性挂线作为确定性手术治疗方法多在直肠推移瓣修补术、LIFT手术等保留括约肌手术失败时使用,因肛门失禁风险大,建议谨慎选择[100]。肛瘘栓治疗瘘管型肛周CD的治愈率为55% ~ 58%,未发现肛门失禁现象[120]。有研究认为肛瘘栓与英夫利西单克隆抗体(infliximab,IFX)联合使用可提升其远期疗效[121]。
9.干细胞局部注射治疗瘘管型肛周CD可能具有良好的应用前景。推荐等级:建议
初步研究证实,间充质干细胞(mesenchymal stem cell,MSC)局部注射治疗瘘管型肛周CD安全有效。自体骨髓MSC可促进瘘管型肛周CD瘘口愈合,自体脂肪来源的干细胞治疗能使57%的瘘口获得愈合,采用其他脂肪来源成分促进瘘口愈合也有报道[122,123,124]。一项多中心三期、双盲、平行、安慰剂对照临床试验观察局部注射脂肪来源的MSC对复杂性瘘管型肛周CD的治疗效果,注射后24周治疗组与安慰剂组症状缓解率分别为49.5%和34.3%[125]。目前尚无MSC局部注射相关不良反应的报道。
10.直肠或结直肠切除、永久性肠造口是难治性肛管直肠病变的最终选择。推荐等级:推荐
对于直肠病变严重的复杂性瘘管型肛周CD、狭窄>4 cm的肛管直肠重度狭窄、肛门失禁和肛周感染导致的难以控制的脓毒血症等情况,如果药物治疗和局部外科干预失败,建议及时行肠造口或直肠切除。肠造口后仅有不到25%的患者能够还纳造口,造口还纳后,肛周炎症常会复发,大多数患者最终需要行直肠切除术[126]。对于全结直肠病变者,全结直肠切除、永久性回肠造口是大多数患者的最终选择。
11.咪唑类和喹诺酮类抗生素有助于控制肛周感染。推荐等级:强烈推荐
咪唑类和喹诺酮类抗生素诱导CD缓解的疗效尚存争议,但可有效控制肛周感染[127]。单独使用环丙沙星4 ~ 12周能够显著减少瘘管引流量[128]。在使用抗生素控制感染的基础上使用免疫调节剂(硫唑嘌呤)有利于瘘管型肛周CD的维持缓解[129]。抗TNF-α单抗联合环丙沙星使用12周,治疗肛瘘有效率可达71%,维持缓解率为65%;而单独使用抗TNF-α单抗组有效率仅有47%,维持缓解率为33%[130]。因此,抗生素常与免疫调节剂或生物制剂联合或序贯使用治疗合并感染的瘘管型肛周CD[99]。
12.推荐在瘘管炎症消失、有愈合趋势时拆除挂线。推荐等级:推荐
肛周瘘管型病变是否采用长期挂线治疗尚有争议,对拆除挂线的时机也无定论。过早拆除挂线,瘘管感染极易复发;拆除过晚,妨碍瘘管愈合[131]。建议挂线至少应维持到IFX诱导缓解结束,并满足以下条件时方可考虑拆线:(1)挂线引流和生物制剂诱导治疗后PDAI显著下降;(2)局部瘘管周围红肿明显消退;(3)瘘管管径明显缩小,冲洗有阻力;(4)按压瘘管无明显脓性分泌物;(5)对比手术前后影像学检查显示炎性病灶明显缩小[100]。为防止挂线意外脱落,对长期挂线者建议每6个月更换1次挂线[132]。
13.肛周CD术后推荐使用有效药物维持缓解,并进行长期随访监测。推荐等级:强烈推荐
肛周CD术后容易复发,合并肛周病变也是CD复发的风险因素,推荐对肛周CD患者使用IFX或巯嘌呤类药物预防复发,并在肛周CD术后定期行直肠指诊、结肠镜、影像学和实验室等检查,监测局部复发和癌变,并为CD维持治疗提供依据[64]。
1.对药物治疗无效的急性重症溃疡性结肠炎,推荐手术治疗。推荐等级:强烈推荐
急性重症溃疡性结肠炎(acute severe ulcerative colitis,ASUC)进展快、病死率高,治疗目的不是挽救结肠,而是挽救生命,应由MDT讨论确定治疗方案,避免延误手术时机。
ASUC静脉激素治疗3 ~ 5 d后应进行疗效评价[133],对效果不佳或无效者推荐药物挽救治疗或直接手术[134];对挽救治疗4 ~ 7 d无显著改善者推荐急诊结肠切除手术[133];部分患者激素治疗失败后行直接手术可缩短术前治疗时间,降低术后并发症发生率及病死率。ASUC并发中毒性巨结肠一旦穿孔,病死率高达57%,强烈推荐尽早手术。
2.对内科治疗疗效不佳的慢性复发型UC推荐及时手术治疗。推荐等级:强烈推荐
慢性复发型UC药物治疗失败(包括生物制剂治疗6周C-反应蛋白未恢复正常,治疗12周未达到黏膜愈合)或反复住院是结肠切除的重要预测因素[135,136]。病变范围广或治疗期间疾病范围逐渐扩大、全身状况恶化(持续贫血或低白蛋白血症伴C-反应蛋白升高)、反复合并艰难梭菌感染(Clostridioides difficile infection或Clostridium difficile infection,CDI)感染[137,138]、药物不良反应或疾病肠外表现导致的生活质量下降、儿童慢性复发型UC导致生长发育障碍均需要及早手术治疗[139,140]。
3.对高龄UC患者如果药物疗效不佳,推荐尽早手术治疗。推荐等级:推荐
高龄(>50岁)患者合并症多,延误最佳手术时机增加病死率,早期择期手术比长期药物治疗可获得更好的生存率和经济学优势[141]。因此,对于高龄或有多个合并症的患者,如预计药物治疗失败的风险较高,建议尽早手术。
4.对长病程UC合并结肠狭窄者,推荐手术治疗。推荐等级:强烈推荐
UC合并狭窄发生率约14.2%[142],其中约10%发生上皮内瘤变或癌变[143]。由于取检困难,且结肠炎相关肿瘤浸润性更强,即使内镜活检为阴性或低级别上皮内瘤变(low grade dysplasia,LGD)也不能排除肿瘤可能,因此对病程长(>8年)的UC合并狭窄,尤其是伴有其他风险因素如原发性硬化性胆管炎(primary sclerosing cholangitis,PSC)、内镜无法通过并准确取活检者,推荐手术治疗。
5.对UC癌变、内镜切除不满意和不适宜内镜切除的上皮内瘤变者推荐手术治疗。推荐等级:强烈推荐
UC合并结直肠癌或上皮内瘤变时,同时性或异时性多源发肿瘤的发生率较高。边界清楚的高级别上皮内瘤变(high grade dysplasia,HGD)首选内镜下切除,并根据切除病理结果决定是否补做结肠切除术或定期随访;非腺瘤样异型增生相关病变或肿物(dysplasia-associated lesion or mass,DALM)的癌变率高,且36% ~ 41%的LGD-DALM术后病理亦为HGD或结直肠癌,因此推荐手术[144]。内镜下不可见(扁平)的HGD有40% ~ 60%已癌变,推荐手术;内镜下不可见(扁平)的LGD应采用手术还是内镜下监测尚无定论,需要患者、内镜医生及结直肠外科医生共同讨论决定。
6.UC择期手术前推荐进行预康复,手术遵循ERAS路径。推荐等级:强烈推荐
对择期手术的UC患者,推荐由MDT制定预康复方案,包括纠正营养不良、撤减激素和生物制剂等。营养治疗首选EN,严重腹泻伴营养不良患者采用禁食、TPN以便控制腹泻症状。遵循ERAS路径可能会降低术后手术部位感染、肠麻痹和吻合口漏的发生率[145,146]。
7.推荐UC手术前尽量撤减或停用激素,但巯嘌呤类、环孢素、他克莫司类药物不影响术后并发症,术前不需要停用。对需急诊手术患者推荐通过损伤控制手术降低并发症风险,不建议因为术前使用抗TNF-α单抗或激素而推迟UC手术。推荐等级:强烈推荐
术前使用抗TNF-α单抗对术后并发症的影响尚不明确[147,148],然而数据显示,在生物制剂时代UC术后病死率增加,尤其是急诊手术[149]。虽然尚难以判定这一现象是抗TNF-α单抗对手术并发症的直接影响,还是使用抗TNF-α单抗使患者病情加重或是手术延迟的结果,但不建议因为使用抗TNF-α单抗或激素而推迟手术。预康复不满意、存在多项手术并发症风险因素或需要急诊手术者,推荐在决定手术后24 h内实施手术,采取三期或改良二期IPAA术式。ASUC手术推迟将显著增加术后并发症及病死率[150]。术前病程短、用药少的患者IPAA术后远期储袋功能更佳[151,152]。
8.推荐IPAA手术作为UC的确定性手术方式,择期IPAA手术推荐分二期进行,对急诊手术或术后并发症风险高者推荐行结肠大部分切除,危急时可采用横结肠造口术。推荐等级:推荐
IPAA手术不但切除UC靶器官,而且在末端回肠构建储袋并与肛管进行吻合,使术后患者生活习惯和生活质量接近正常,是目前推荐的UC根治性手术方式。
IPAA可分一期、二期(包括改良二期)和三期进行:
一期IPAA:一次手术完成全结直肠切除+IPAA,无保护性造口,适用于经过严格筛选的一般状况良好、直肠炎症较轻、无手术并发症风险因素的患者。
二期IPAA:是推荐的择期手术方式,第一次手术完成全结直肠切除+IPAA,并在储袋近端行转流性回肠造口,术后8周左右进行第二次手术,将造口还纳。
三期IPAA:适用于ASUC、术后并发症风险高或急性重症结肠炎诊断不明确(IBD未定型或缺血性结肠炎时先行结肠次全切除术,待术后病理诊断明确并与患者充分沟通后再决定是否实施IPAA)者。三期IPAA的第一次手术行结肠次全切除+回肠造口,第二次手术切除残余结直肠并构建储袋+转流性回肠造口,第三次手术行回肠造口还纳。三期IPAA手术的优势主要体现在提高第一期手术的安全性,不足之处是第一期手术后残留结直肠可能存在持续性炎症或残端开裂、术后肠系膜纤维化挛缩、第二期手术时中转开放手术比例增加等,整体并发症发生率并不低于甚至高于二期IPAA,远期结局也无优势[153]。因此,对药物治疗失败者应果断决策、早期手术,争取行二期IPAA[154];无重建手术意愿和(或)有禁忌证(如括约肌功能不全、肛周病变)者也可选择结肠次全切除+回肠造口术,残留直肠炎可采用药物或内镜等治疗手段[155,156]。
改良二期IPAA:第一次手术行结肠次全切除及回肠造口,第二次手术切除残余结直肠并行IPAA,但不行转流性回肠造口。与经典二期手术相比,改良二期手术可能不增加甚至减少吻合口漏和术后肠梗阻的风险[157],但关于改良二期IPAA对储袋远期功能影响的研究较少。
对于中毒性巨结肠或妊娠期ASUC等危重患者,可以仅行横结肠造口或加行回肠造口控制病情,待病情稳定后再行IPAA手术[158]。
9.对儿童和青少年UC如果有手术指征,首选IPAA手术。推荐等级:推荐
儿童和青少年患者实施IPAA术后并发症和储袋失败率较低,远期功能良好,与成人患者并无差异[159]。采用腹腔镜实施IPAA手术能够减少儿童和青少年患者手术并发症,缩短住院时间。
10.对高龄患者可以实施IPAA手术。推荐等级:推荐
单纯高龄不是不能行IPAA手术的理由。虽然高龄(>50岁)患者较年轻患者IPAA术后近期并发症有所增加,脱水风险加大,术后住院时间延长,术后1 ~ 2年内排便失禁发生率也高于年轻人,但采用双吻合技术(double stapling technique,DST)能够减少括约肌损伤风险,远期储袋功能与年轻患者差别不大[160]。
11.对合并PSC患者实施IPAA手术的远期储袋失败风险增加。推荐等级:推荐
合并PSC的UC患者实施IPAA术后储袋失败率高于非PSC患者,储袋功能也不如非PSC患者,储袋炎发生率增加[161]。对于需要肝脏移植的PSC患者,结肠切除+永久性末端回肠造口比IPAA更有利于维持移植器官远期功能[162]。
12.对UC合并癌变或HGD者可以实施IPAA手术,但推荐按照肿瘤外科原则进行。推荐等级:强烈推荐
术前合并癌变或HGD、需要手术的UC患者,可以行IPAA手术,并按照肿瘤外科原则切除系膜并清扫淋巴结,部分直肠病变轻微的结肠HGD可考虑实施回直肠吻合术(ileorectal anastomosis,IRA);合并低位直肠HGD或者早期癌变者,可以行全系膜切除(total mesorectal excision,TME)、直肠黏膜剥除或经肛内括约肌切除术(intersphincteric resection,ISR)+IPAA。既往有结直肠肿瘤的患者在IPAA手术后储袋肿瘤风险增加[163]。
进展期直肠肿瘤实施IPAA手术要权衡利弊,如果需要进行放疗,建议术前进行。但即使术前进行放疗,也会增加储袋吻合口漏和腹泻风险,建议实施保护性回肠造口术。储袋手术后实施放疗极可能导致储袋失败。
13.IPAA手术切除直肠时,推荐采用改良TME术式。推荐等级:推荐
在排除HGD或癌变的前提下,手术切除直肠采用贴近直肠或TME方式均可,推荐采用改良TME术式(前侧方在Denovillier筋膜后方贴近肠管处游离以保护自主神经,后方按照TME原则进行)。
贴近直肠切除的理论优势是减少盆腔自主神经损伤的风险,保留的直肠系膜能填充盆腔,对储袋起到支撑作用,术后即使发生吻合口漏,也可减少慢性窦道形成的风险。但保留直肠系膜对储袋远期功能的影响尚不明确。储袋周围脂肪炎症可能与储袋炎及储袋功能不佳有关[164]。
14.储袋肛管吻合要确保无张力,必要时行系膜延长。推荐等级:强烈推荐
吻合无张力和血供良好对IPAA手术成功至关重要,对于肥胖、腹腔多次手术者,更应该警惕吻合口张力问题。为保证吻合口无张力,游离小肠系膜可达十二指肠水平部,但也不宜过度松弛,以免引起储袋松弛综合征。采用DST吻合时,储袋顶端至少超过耻骨结节下缘2 ~ 3 cm;采用手工吻合时,储袋顶端超过耻骨结节下缘5 ~ 6 cm。吻合前要认真检查系膜方向,确定储袋无扭转。预计吻合张力大时,可以尝试如下方法:根据回结肠血管走行适当裁剪血管弓[165];垂直肠系膜上血管走行方向在脏层腹膜前后页作数个横行切口;保留右结肠动脉和边缘动脉弓,切断回结肠和末端回肠血管;采用S型储袋较J型储袋可额外延长系膜2 ~ 3 cm。
15.推荐规范实施储袋手术,首选J型储袋。推荐等级:强烈推荐
良好的储袋功能取决于完善的括约肌功能、协调的排便反射、足够的储袋容积和良好的顺应性。此外,储袋制作经验对储袋功能影响较大。常用储袋形状包括J型、S型和H型,也有D型储袋的报道[166]。J型储袋制作简单,易于排空,远期功能与其他储袋无差异,推荐作为首选的储袋形状;S或H型储袋可作为储袋失败后重建手术或因储袋肛管吻合张力大而需要手工吻合时选用。J型储袋长度推荐为15 ~ 20 cm,S型储袋每个臂长度推荐为12 ~ 15 cm,流出道不应长于2 cm,否则易引起输出袢综合征和排便困难[167]。
16.推荐采用DST进行储袋肛管吻合,吻合口距齿状线不应超过2 cm。推荐等级:推荐
回肠储袋与肛管的吻合方式有两种,包括传统术式和DST。传统术式是将齿状线以上的肛管移行区(anal transitional zone,ATZ)黏膜剥除,仅保留移行区肌鞘,再将储袋套入肌鞘,与齿状线缝合。但实际操作时黏膜剥除往往不完全,残留的黏膜被储袋覆盖,容易掩盖上皮内瘤变或癌变。另一方式是采用DST,在距离齿状线2 cm以内将储袋与肛管吻合。该术式操作简单,保留了肛管移行区,术后控便能力、肛管静息压及直肠肛管抑制反射(与夜间污粪有关)均优于传统术式[168],而盆腔感染、术后肠梗阻和吻合口狭窄等发生率下降,是推荐的储袋肛管吻合方式。两种术式术后移行区肿瘤发生率差异并无统计学意义,当肛管移行区明确存在上皮内瘤变或因其他原因(如肛管狭窄)无法实施DST时,可考虑行传统术式。
17.推荐IPAA术后8 ~ 12周还纳造口,还纳前对储袋进行评估。推荐等级:强烈推荐
转流性造口的还纳时间一般为储袋手术后8 ~ 12周,时间过久增加术后肠麻痹的风险[169]。部分条件较好的患者如果储袋术后无吻合口漏的相关症状,影像学或内镜检查正常,可考虑术后2周内还纳造口[170]。造口还纳可采用手工或器械吻合,器械吻合耗时较短。
造口还纳前需要对储袋进行评估,储袋造影的敏感性不及病史及麻醉下肛门探查,不作常规推荐。以下情况推荐实施储袋造影检查:患者有吻合口漏相关的临床症状和体征,或者虽然无症状,但直肠指诊或储袋镜提示吻合口异常[171]。如果储袋造影发现造影剂外渗,需及时处理。
18.推荐采用腹腔镜行择期IPAA术,有条件的中心可考虑机器人手术。推荐等级:推荐
腹腔镜手术虽然延长手术时间,增加治疗费用,但可以减轻腹腔粘连,降低并发症发生率,缩短住院时间,改善术后短期结局,获得更好的储袋远期功能和生育功能。儿童患者采用腹腔镜手术也能减少术后短期并发症,缩短住院时间。机器人IPAA可获得与腹腔镜手术类似的近期结局,但其临床优势仍需更多前瞻性研究证实,在有经验的中心可以考虑尝试[172]。
与单纯腹腔镜手术相比,经肛微创IPAA手术(trans-anal minimally invasive surgery-IPAA,TAMIS-IPAA)由两组术者配合,经腹经肛同时操作,能缩短手术时间;直视下切断直肠能够避免直肠残留过多和封套炎风险;经肛手术切除直肠方便,能够降低三期IPAA手术难度,尤其是旷置直肠出现残端漏时的手术难度[173];TAMIS-IPAA在储袋重建(redo pouch)手术中也有较为明显的优势[174]。
19.行急诊手术时,推荐根据病情选择微创或开放手术。推荐等级:强烈推荐
在有经验的中心,对ASUC患者行腹腔镜下急诊结肠切除可以缩短术后住院时间,减少感染性并发症。但当ASUC继发中毒性巨结肠、肠穿孔、严重大出血或患者状况危重(ASA>3级)时,应以争取时间、抢救生命为主,强烈推荐采用开放手术。
20.对育龄期UC患者推荐采取个体化的手术方案以降低不孕的风险。推荐等级:强烈推荐
影响男性UC患者生育功能的主要因素包括活动性UC和手术对性功能的影响。活动期UC本身可以造成性功能下降,IPAA手术消除UC症状,有助于改善男性性功能。盆腔手术和直肠切除虽有导致性功能障碍的风险,但随着腔镜技术的进步和神经保护认识的加深,这一风险正在降低,总体上讲,IPAA可提高男性UC患者的性功能和术后生育率[175]。
与男性不同,影响女性UC患者生育功能的最主要因素是IPAA手术操作造成的盆腔和输卵管粘连、堵塞及疤痕形成。腹腔镜IPAA可以减轻盆腔粘连,降低女性不孕率,缩短受孕时间[176],但不孕风险仍未消除。近期备孕的女性如果有手术指征,可以先行回直肠吻合术或结肠次全切除手术,完成生育后再实施IPAA手术。对IPAA术后不孕女性,推荐实施体外受精(in vitro fertilization,IVF)技术[177]。
21.UC患者回直肠吻合术后残留直肠发生顽固性炎症和癌变的概率高,最终需要切除直肠,切除时推荐经括约肌间直肠切除术。推荐等级:推荐
回直肠吻合操作相对简单,术后并发症、排便频率和夜间漏便现象以及对生育功能的影响可能优于IPAA,但术后10年失败率达27%,术前免疫调节剂或抗TNF-α单抗治疗无效者失败风险更高,失败的主要原因为顽固性直肠炎[178]。回直肠吻合远期癌变率高,术后20年残留直肠发生上皮内瘤变和癌变的概率分别为14%和7.3%[179],20.8%患者需要切除直肠[178]。切除时推荐采用经肛内括约肌切除术式,以保留盆底肌肉群及外括约肌,减少会阴切口愈合不良的风险。
经与患者及家属充分交流后,回直肠吻合可以用于以下患者:直肠病变轻微、局部药物治疗有效、术后随访依从性好的HGD或结直肠癌患者;作为育龄期患者IPAA的桥接术式;肛门括约肌功能较差但直肠病变轻微的老年患者;或病理未能获得明确诊断(怀疑未定型肠炎或CD)者。
22.要重视预防ASUC急诊手术后并发症,早期手术是提高疗效的关键。推荐等级:推荐
ASUC急诊手术病死率为5.3% ~ 12.9%,并发症发病率为15% ~ 65%[180],主要并发症包括直肠残端开裂、出血、盆腔脓肿、术后延迟性肠麻痹等,少见但病死率高的并发症还有弥漫性小肠炎等。高龄(>50岁)、急诊手术及医生缺乏急诊手术经验是ASUC术后高病死率的独立风险因素[181,182]。
采用有限结肠镜(乙状结肠镜)、粪钙卫蛋白(fecal calprotectin)检测、CT或MRI等手段早期预测ASUC对药物治疗的反应,避免因无效的药物治疗延误手术时机是减少术后并发症和降低病死率的关键[150]。
23.ASUC行结肠次全切除时,不建议将结直肠残端留在腹腔。推荐等级:推荐
ASUC行结肠次全切除+末端回肠造口术时,直肠残端并发症发生率较高,主要为活动性直肠炎及其导致的残端开裂。虽然残留的直肠仍可能有活动性炎症甚至出血,但如果为尽量去除病变肠段而将直肠残端保留过短(断端在腹膜返折以下),不仅增加后期直肠切除难度和神经损伤的风险,而且发生残端漏和盆腔感染后处理非常困难[183]。推荐在切除结肠的同时适当保留乙状结肠远端以便将残端外置造口,或封闭后埋于皮下[184]。如果结肠残端留置于腹腔,建议在直肠内放置经肛门引流管。
24.推荐IPAA术后储袋吻合口瘘尽早干预,以降低储袋失败的风险。推荐等级:强烈推荐
储袋并发症(如储袋漏或窦道形成等)是导致储袋失败的重要原因。IPAA术后盆腔脓肿和吻合口漏的发生率为6% ~ 16.8%。肥胖、术前使用激素时间过长、吻合有张力及血供不佳、围手术期输血是IPAA术后早期盆腔脓肿和吻合口漏的风险因素[185,186]。吻合口漏的最常见部位是储袋肛管吻合口,其次是储袋顶端。盆腔脓肿等并发症可引起储袋周围瘢痕形成、顺应性下降、远期储袋功能降低,也是导致储袋失败的重要原因[187]。
IPAA术后怀疑储袋吻合口并发症时推荐及早干预,水溶性造影剂灌肠后盆腔CT是吻合口漏的首选诊断手段。吻合口漏相关的盆腔脓肿首选麻醉下肛门探查引导下经肛门置入引流管,通过漏口置入脓腔[188];内镜下海绵辅助真空闭合(endoscopic vacuum assisted closure,endo-VAC)技术较传统治疗能使脓腔更快消失,更好地保留储袋功能[189];吻合口缺损较大时,推荐全麻下经肛门进行修补[190]。储袋手术时未转流患者,储袋瘘诊断明确后建议行回肠袢式造口,合并弥漫性腹膜炎者建议腹腔冲洗引流,储袋顶端瘘可采用内镜下夹闭技术(over-the-scope clip,OTSC)[191]。未找到漏口的盆腔脓肿建议使用广谱抗生素和影像学引导下经皮穿刺引流。经过充分引流,多数漏口可闭合,长期不愈合的漏口可能需要内镜治疗、储袋修复或重建。
25.对IPAA术后储袋出血推荐局部处理或内镜止血。推荐等级:强烈推荐
IPAA术后储袋出血多出现在术后24 h内[192],最常见部位为储袋肛管吻合口。血流动力学稳定的储袋内出血可采用肾上腺素溶液局部冲洗,出血量大或血流动力学不稳定者推荐行储袋内镜检查,吻合线出血可夹闭,弥漫性渗血采用去甲肾上腺素灌肠,术后晚期储袋出血需警惕吻合口漏可能。制作储袋时加强缝合、吻合器延时击发、击发后观察数分钟或将储袋翻转检查吻合线等有助于止血,必要时在储袋肛管吻合完成后进行内镜检查,可以早期发现并处理活动性出血。
26.IPAA术后肠梗阻常见,多数患者可通过非手术治疗获得缓解。推荐等级:推荐
IPAA术后30 d内肠梗阻发生率为21.9% ~ 25.8%。远期肠梗阻的发生率为10% ~ 30%[193],腹腔镜手术能否降低肠梗阻发生率仍有争议[194]。IPAA术后30 d内的肠梗阻多可通过非手术治疗获得缓解,但约1/4的肠梗阻患者最终需要手术治疗,反复发作的肠梗阻推荐手术治疗。对造口还纳前发生过肠梗阻的患者,还纳时推荐实施腹腔探查和粘连松解。
27.UC术后静脉血栓风险增加,推荐预防性抗凝治疗。推荐等级:强烈推荐
UC术后静脉血栓栓塞(VTE)发生率为2.74% ~ 4.30%,显著高于其他结直肠疾病[195],术后门静脉血栓形成的风险也较高(8.3%)[196]。急诊手术、高危择期手术、术前使用激素和低蛋白血症是术后VTE的风险因素。要重视UC术后早期下床活动,除非有禁忌证,推荐UC术后第2天开始抗凝治疗直至出院,高危患者延长抗凝时间至术后4周以上,其他预防VTE措施包括使用梯度加压治疗仪和弹力袜等。
28.对IPAA术后的女性患者要谨慎选择分娩方式。推荐等级:强烈推荐
IPAA术后经阴道分娩有导致括约肌撕裂的风险,对远期储袋和控便功能造成不利影响。患者在分娩前,需要与结直肠外科和妇产科医生共同商量决定分娩方式,首选剖宫产。对高危产妇(可能需要产钳助产、会阴侧切、巨大儿、第二产程超过2 h等)强烈推荐剖宫产[197]。
29.对IPAA术后储袋炎或封套炎首选药物治疗。推荐等级:强烈推荐
约50%的UC患者在IPAA术后发生储袋炎,其中40%在术后第1年发生[198]。储袋炎的一线治疗方案为甲硝唑、环丙沙星或利福昔明,可加用布地奈德。严重或慢性顽固性储袋炎(尤其是CD样储袋炎)可使用抗TNF-α单抗或其他生物制剂[199]。美沙拉嗪栓剂为封套炎的一线治疗药物,残留直肠封套过长(>2 cm)且症状较重者可考虑储袋重建手术。
30.对药物治疗无效的储袋炎和储袋复杂并发症推荐手术治疗。推荐等级:强烈推荐
约10%的储袋失败由慢性储袋炎引起,药物治疗无效者推荐手术治疗,但手术方案仍无定论,储袋切除+回肠造口术虽然较单纯的转流性造口难度大,术后可能残留会阴部窦道,但术后生活质量更佳[200]。
储袋慢性窦道或储袋瘘是远期储袋失败的最主要原因。慢性窦道的手术方式包括黏膜瓣推移、储袋整体前移、储袋重建等,但仍有约1/3的患者最终需要永久性回肠造口甚至切除储袋。部分患者采用内镜下针刀窦道切开术(endoscopic needle knife sinusotomy,NKSi)可以获得良好的疗效,从而避免手术[201]。
储袋瘘包括储袋阴道瘘、储袋会阴瘘等,储袋阴道瘘相对常见。术后早期的储袋阴道瘘多与外科并发症有关,术后1年以上发生者要排除储袋CD。储袋阴道瘘的处理取决于病因、症状严重程度、治疗时机及个体解剖。炎症活动期或合并脓肿时先行引流和挂线,确定性手术修补前建议先行转流。手术方案包括肛瘘栓、经阴道和经肛门修补、储袋推移瓣和储袋重建等。储袋瘘远期预后不佳,约70%的患者最终需行回肠造口。
储袋肛管吻合口狭窄可由外科并发症或储袋周围感染引起,治疗上首选各种扩张技术或内镜下针刀治疗,无效时再行手术。储袋近端回肠狭窄建议排除CD,对储袋近端长度<4 cm的纤维性狭窄推荐内镜扩张或针刀治疗,>4 cm或多发的输入袢狭窄推荐狭窄成形术[202]。
其他复杂的外科并发症如输入袢综合征、输出袢综合征、储袋脱垂、储袋前突、巨型储袋和储袋扭转等多需要手术纠正或行储袋重建手术[203,204]。
储袋重建手术操作复杂,并发症风险高,5年成功率低于初次储袋手术[205],仅限于在经验丰富的IBD中心实施,具有明确的手术适应证和手术预案、手术意愿强烈并做好充分术前准备的患者可以取得较好的治疗效果[206]。具有非感染性并发症的患者行储袋重建手术的远期效果优于感染性并发症患者。
31.推荐对UC术后残留的直肠炎进行治疗和定期内镜监测。推荐等级:强烈推荐
UC术后残留的直肠炎和封套炎患者需要药物维持缓解治疗。由于残留直肠黏膜有癌变的风险,需要定期内镜监测。
内镜监测方案:(1)病程<20年者,无需监测;(2)病程>20年者,每5年1次;(3)合并PSC或者既往结直肠上皮内瘤变者,每2 ~ 3年1次;(4)存在高风险因素(发病年龄<20岁且病史>10年,或合并结直肠癌)者,每年1次[207]。
32.对具有储袋相关并发症者需进行储袋镜检查,对具有储袋癌变风险因素的患者推荐定期进行储袋监测。推荐等级:强烈推荐
IPAA术后1年内出现的储袋炎需要与储袋相关外科并发症(如慢性窦道、盆腔脓肿、储袋机械并发症)相鉴别,还要与储袋CD、封套炎、储袋易激综合征、储袋前末端回肠炎等其他情况相鉴别。储袋炎患者艰难梭菌感染发生率高,推荐进行检测。储袋术后癌变率为1.2% ~ 1.8%,风险因素包括慢性储袋炎或封套炎、储袋活检提示黏膜萎缩和固有层明显炎症、一级亲属患结直肠癌或PSC等[208]。
内镜是储袋炎最重要的诊断手段,检查时除观察储袋体外,还应仔细观察储袋近端末端回肠及肛管移行区,单纯的储袋吻合线溃疡而其他部位黏膜正常者不能诊断为储袋炎。储袋镜可以每年检查1次,根据检查结果再决定储袋镜检查频次;也可以根据癌变风险因素进行风险分层,安排储袋镜检查及活检方案:(1)无风险因素,UC病程10年以上,每1 ~ 3年1次;(2)有风险因素者,每1 ~ 2年1次;(3)术前有结直肠癌病史,每年1次[209]。
综上所述,IBD是一种病因仍不明确的内科疾病,虽然目前无法避免外科手术,但早期诊断、积极治疗活动性炎症、长期维持疾病缓解能够降低手术率。外科治疗极其重要,其宗旨是解决内科治疗无效的IBD肠道并发症,恢复肠道正常结构,提高患者生活质量。MDT是治疗IBD最主要的组织形式,综合各学科的先进技术、结合最新的内外科治疗理念将极大地提高IBD治疗效果和患者满意度。
执笔者名单(按撰写任务量排序)
CD:李毅,朱维铭,柯嘉,周伟
肛周CD:谷云飞,李悠然,朱维铭
UC:龚剑峰,朱维铭,吴斌,杜鹏
投票专家(按姓氏汉语拼音排序):曹倩(浙江大学医学院附属邵逸夫医院),陈春球(同济大学附属第十人民医院),陈旻湖(中山大学附属第一医院),崔喆(上海交通大学医学院附属仁济医院),丁召(武汉大学中南医院),杜鹏(上海交通大学医学院附属新华医院),高翔(中山大学附属第六医院),龚剑峰(解放军东部战区总医院),谷云飞(江苏省中医院),韩方海(中山大学孙逸仙纪念医院),韩英(解放军总医院第七医学中心),何子锐(上海交通大学医学院附属瑞金医院),胡品津(中山大学附属第六医院),黄忠诚(湖南省人民医院),蒋小华(上海同济大学附属东方医院南院),柯嘉(中山大学附属第六医院),兰平(中山大学附属第六医院),李毅(解放军东部战区总医院),李永翔(安徽医科大学第一附属医院),刘刚(天津医科大学总医院),刘玉兰(北京大学人民医院),刘占举(同济大学附属第十人民医院),卢云(青岛大学附属医院),鲁明典(安徽医科大学第一附属医院高新区院区),孟文建(四川大学华西医院),缪应雷(昆明医科大学第一附属医院),钱家鸣(北京协和医院),钱群(武汉大学中南医院),冉志华(上海交通大学医学院附属仁济医院),申占龙(北京大学人民医院),邰建东(吉林大学白求恩第一医院),王大广(吉林大学白求恩第一医院),王金海(浙江大学医学院附属第一医院),王玉芳(四川大学华西医院),王自强(四川大学华西医院),吴斌(北京协和医院),吴开春(空军军医大学西京消化病医院),吴小剑(中山大学附属第六医院),吴小平(中南大学湘雅二医院),向开敏(中南大学湘雅三医院),肖卫东(陆军军医大学附属新桥医院),徐栋(浙江大学医学院附属第二医院),姚宏伟(北京友谊医院),曾玉剑(昆明医科大学第一附属医院),张卫(海军军医大学长海医院),钟捷(上海交通大学医学院附属瑞金医院),周伟(浙江大学医学院附属邵逸夫医院),朱维铭(解放军东部战区总医院)
黎介寿院士对本共识的完成给予极大的关心,并进行仔细的审读,在此表示衷心感谢!南京大学医学院黄良宇博士为本共识的文献整理花费大量时间,在此深表感谢!
所有作者均声明不存在利益冲突


























