
To prevent risk of life-threatening stent thrombosis, all patients need to undergo dual antiplatelet therapy (DAPT) for at least 6 weeks to 12 months after stent implantation. If DAPT is continued during noncardiac surgery, there is a risk of severe bleeding at the surgical site. Our study was to assess the risk of bleeding in patients with continued DAPT during orthopedic surgery.
The clinical data of 78 patients with coronary heart disease who underwent orthopedic surgery from February 2006 to July 2018 were retrospectively analyzed. Prior to orthopedic surgery, DAPT was continued in 16 patients (group I), 24 patients were treated with single antiplatelet therapy (group II), and 26 patients received low-molecular-weight heparin therapy for more than 5 days after the discontinuation of all antiplatelet therapies (group III). Twelve patients were excluded, as they had undergone minimally invasive surgery such as transforaminal endoscopy and vertebroplasty. The perioperative blood loss of each patient was calculated using Nadler’s formula and Gross’ formula. The intraoperative bleeding volume, total volume of intraoperative bleeding in addition to postoperative drainage, and total blood loss were compared between groups. The level of significance was set at P < 0.05.
There were no significant differences between the three groups in age, intraoperative bleeding volume, total volume of intraoperative bleeding in addition to postoperative drainage, and total perioperative blood loss calculated by Nadler’s formula and Gross’ formula (all P > 0.05). Six patients experienced postoperative cardiovascular complications due to the delayed restart of antiplatelet therapy; one of these patients in group III died from myocardial infarction.
Continued DAPT or single antiplatelet treatment during orthopedic surgery does not increase the total intraoperative and perioperative bleeding compared with switching from antiplatelet therapy to low-molecular-weight heparin. However, the discontinuation of antiplatelet therapy increases the risk of serious cardiac complications.

版权归中华医学会所有。
未经授权,不得转载、摘编本刊文章,不得使用本刊的版式设计。
除非特别声明,本刊刊出的所有文章不代表中华医学会和本刊编委会的观点。
Percutaneous coronary intervention (PCI) is one of the mainstream treatments for coronary atherosclerotic heart disease; it is estimated that millions of stents are implanted worldwide annually.[1] To prevent stent thrombosis, all patients need to undergo dual antiplatelet therapy (DAPT) for at least 6 weeks to 12 months after stent implantation.[2,3] If DAPT is continued during noncardiac surgery, there is a risk of severe bleeding at the surgical site[4]; however, if DAPT is stopped, there is a risk of life-threatening stent thrombosis. Few studies have explored how to balance the risks of bleeding versus thrombosis in patients receiving DAPT who require orthopedic surgery. The current study was designed to assess the risk of bleeding in patients with continued DAPT during orthopedic surgery.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Beijing Anzhen Hospital. The requirement for informed consent was waived by the Ethics Committee of Beijing Anzhen Hospital due to the retrospective nature of the study.
The clinical data from 78 patients with coronary heart disease who underwent orthopedic surgery from February 2006 to July 2018 were retrospectively analyzed. Twelve patients who had undergone minimally invasive surgery (such as transforaminal endoscopy and vertebroplasty) were excluded. The remaining patients were divided into three groups in accordance with the perioperative use of antiplatelet drugs: in group I, DAPT (75 mg/d of clopidogrel and 100 mg/d of aspirin) was continued throughout the perioperative period; group II were receiving single antiplatelet therapy preoperatively or were switched from DAPT to single antiplatelet therapy (100 mg/d of aspirin); in group III, all antiplatelet therapy was suspended and low-molecular-weight heparin therapy was administered for more than 5 days preoperatively. Age, intraoperative bleeding volume, postoperative drainage volume, pre- and postoperative hematocrit values, body height, body weight, and cardiovascular complications were recorded. The total bleeding volume (intraoperative bleeding volume and postoperative drainage) was calculated. The total perioperative blood loss of each patient was calculated using Nadler’s formula and Gross’ formula.
Nadler’s formula for men: PBV = 0.3669 × H3 + 0.03219 × W + 0.6041; Nadler’s formula for women: PBV = 0.3561 × H3 + 0.03308 × W + 0.1833, where PBV is the patient’s blood volume in L, H is the patient’s height in m, and W is the body weight in kg.[5]
Gross’ formula: VL = 1000 × PBV × (H0-HF)/(HO + HF)/2, where PBV is the patient’s blood volume in L, VL is the blood loss in mL, H0 is the patient’s initial hematocrit value, and HF is the patient’s minimum hematocrit value.[6]
The SPSS software package (version 19; IBM Corporation, Armonk, NY, USA) was used for the statistical analyses of intergroup differences in age, intraoperative blood loss, total bleeding volume, and total blood loss. All data are presented as the mean ± standard deviation. As these data were not normally distributed, the Kruskal-Wallis test for independent samples was applied. A P value of <0.05 was considered statistically significant.
Data from a total of 66 patients (33 men and 33 women; mean age 69.1 ± 8.5 years, range 48–87 years) were analyzed, including 16 patients (24.2%) in group I, 24 (36.4%) in group II, and 26 (39.4%) in group III. Of the 66 included patients, 35 (53.0%) underwent spinal surgery or knee or hip replacement surgery [Table 1].
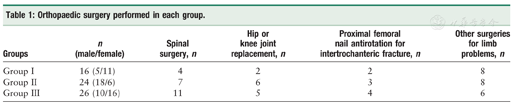
Orthopaedic surgery performed in each group.
Orthopaedic surgery performed in each group.
| Groups | n (male/female) | Spinal surgery, n | Hip or knee joint replacement, n | Proximal femoral nail antirotation for intertrochanteric fracture, n | Other surgeries for limb problems, n |
|---|---|---|---|---|---|
| Group I | 16 (5/11) | 4 | 2 | 2 | 8 |
| Group II | 24 (18/6) | 7 | 6 | 3 | 8 |
| Group III | 26 (10/16) | 11 | 5 | 4 | 6 |
Table 2 summarizes the number of patients, age, and blood loss in the three groups. There were no significant differences between the three groups in patient age (P = 0.428), intraoperative bleeding volume (P = 0.641), total volume of intraoperative blood loss and postoperative drainage (P = 0.483), and total perioperative blood loss calculated by Nadler’s formula and Gross’ formula (P = 0.485).
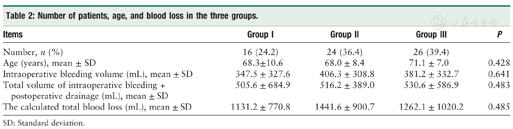
Number of patients, age, and blood loss in the three groups.
Number of patients, age, and blood loss in the three groups.
| Items | Group I | Group II | Group III | P |
|---|---|---|---|---|
| Number, n (%) | 16 (24.2) | 24 (36.4) | 26 (39.4) | |
| Age (years), mean ± SD | 68.3±10.6 | 68.0 ± 8.4 | 71.1 ± 7.0 | 0.428 |
| Intraoperative bleeding volume (mL), mean ± SD | 347.5 ± 327.6 | 406.3 ± 308.8 | 381.2 ± 332.7 | 0.641 |
| Total volume of intraoperative bleeding + postoperative drainage (mL), mean ± SD | 505.6 ± 684.9 | 516.2 ± 389.0 | 530.6 ± 586.9 | 0.483 |
| The calculated total blood loss (mL), mean ± SD | 1131.2 ± 770.8 | 1441.6 ± 900.7 | 1262.1 ± 1020.2 | 0.485 |
SD: Standard deviation.
Two patients developed acute coronary syndrome (ACS) postoperatively. A 64-year-old male patient who had undergone posterior decompression, interbody fusion, and internal fixation for single-segmental lumbar spinal stenosis developed ACS at 39 h postoperatively; his intraoperative bleeding volume was 500 mL, drainage volume within 4 days postoperatively was 660 mL, and calculated total blood loss was 1293 mL. A 63-year-old women who had undergone total hip arthroplasty for right femoral neck fracture developed ACS at 1 week postoperatively; her intraoperative bleeding volume was 300 mL, no drainage tube was placed, and the calculated total blood loss was 1281 mL. ACS was resolved by medications in both cases.
One patient underwent surgery via the anterior approach for C4-C5 tuberculosis and incomplete paralysis. The intraoperative bleeding volume was 200 mL, and the postoperative drainage volume was 50 mL. Nine days postoperatively, a delayed cervical hematoma measuring 4 cm × 6 cm was found; this hematoma did not affect the patient’s respiration, and spontaneously resolved. The calculated blood loss in this patient was 419 mL.
A 51-year-old male patient had a small amount of bleeding from the incision after open reduction and internal fixation of a pilon fracture; the total blood loss was 336 mL.
A 74-year-old female patient was admitted to the hospital 140 days after coronary angiography and was treated with DAPT for 2 days after fracturing the left femoral neck. Deep venous thrombosis of the lower extremity was detected, and the treatment strategy was switched to aspirin (100 mg/day) and low-molecular-weight heparin (Fraxiparine; 0.6 mL subcutaneously every 12 h). After 12 days of treatment, hemiarthroplasty was performed. The intraoperative blood loss was 300 mL, and no drainage tube was placed. ACS occurred late in the operation and was treated with medications. Aspirin combined with Fraxiparine was resumed the next day, and there was a large amount of bleeding from the incision. The calculated total blood loss was 3341 mL.
Postoperative cardiac complications occurred in three patients, one of whom died. The deceased patient was a 58-year-old female patient who had started DAPT after coronary stenting. Five days later, she developed a right-sided Colles’ fracture. The DAPT was then replaced by Fraxiparine (0.6 mL subcutaneously every 12 h). Six days after stent implantation, the patient underwent open reduction and internal fixation of the distal radius fracture, with the application of a tourniquet on the forearm. Nine hours postoperatively, the patient experienced sudden cardiac pain and cardiac arrest, and died before the administration of any antiplatelet and/or anticoagulant therapy.
A 68-year-old female patient had been treated with oral aspirin for 8 years after stent implantation. Before spinal surgery, the aspirin was discontinued, and 0.4 mL of Fraxiparine® was injected subcutaneously every 12 h. Nine days later, the patient underwent posterior decompression of the lumbar spinal canal, internal fixation with pedicle screws, and interbody fusion at L4-S1. ACS was detected 27 h postoperatively and was alleviated after sublingual administration of nitroglycerin and oral administration of aspirin. The intraoperative bleeding volume was 500 mL, of which 200 mL was salvaged intraoperatively. The total drainage volume was 220 mL within the first 5 days postoperatively. A total of 800 mL of allogeneic blood was transfused. The calculated total blood loss was 1486 mL.
A 78-year-old female patient had coronary heart disease but did not undergo stent placement. She had 2-year history of oral administration of DAPT comprising clopidogrel and aspirin. After an intertrochanteric fracture of the right femur, the DAPT was suspended for 5 days. The patient then underwent closed reduction and internal fixation with proximal femoral nails. ACS occurred 2 days postoperatively and was alleviated by oral medications (clopidogrel and aspirin, and low-molecular-weight heparin calcium at a dosage of 4100 IU subcutaneously every 12 h). The intraoperative bleeding volume was 600 mL, calculated total blood loss was 3763 mL, and volume of allogeneic blood transfused was 1400 mL.
There were no complications due to intraspinal hematoma compression of spinal nerves in our series.
When a patient requires noncardiac surgery in the early period after commencing DAPT after coronary stenting, stopping the antithrombotic therapy can increase the risk of serious adverse cardiac events due to stent thrombosis. However, continuing antiplatelet therapy during the perioperative period may increase the risk of bleeding at the surgical site.[7,8]
The reported incidences of perioperative cardiac events during noncardiac surgery performed after bare metal stent implantation are 10.8% for surgery performed within 30 days, 3.8% for surgery performed within 31 to 90 days, and 2.8% for surgery performed more than 91 days after stent implantation.[9] For drug-eluting stents, the incidence of cardiac events is 11.6% for surgery performed within 6 weeks after stenting; however, the incidence decreases to 6.4%, 4.2%, and 3.5% when the interval between stenting and surgery is 6 weeks to 6 months, 6 to 12 months, and 12 to 24 months, respectively.[10] Therefore, international guidelines recommend that non-cardiac surgery should be performed at least 6 weeks after cardiac stenting, and preferably 6 months later; however, for patients at high risk of ACS, elective surgery should be postponed until 1 year after stenting due to the high risk of thrombosis, regardless of the type of stent used.[11,12]
Sudden spinal cord or cauda equina compression in a patient with spinal disease can lead to paraplegia or severe spinal nerve dysfunction; thus, emergency surgery or early surgery is often required.[13,14] Patients receiving uninterrupted DAPT are at high risk of massive intraspinal hemorrhage after spinal surgery, and hematoma compression of the spinal cord or cauda equina nerve can lead to catastrophic consequences.[15,16] In addition, the current aging society has resulted in a high incidence of hip fracture among older adults.[17] Many studies have confirmed that surgical treatment within 48 h after fracture significantly decreases complications and mortality,[18,19] as recommended by multiple guidelines. However, the European Society of Cardiology (ESC)/European Society of Anaesthesiology (ESA) guidelines developed in 2014 suggest that antiplatelet therapy should be discontinued more than 5 to 7 days before noncardiac surgery,[12] which obviously conflicts with the recommendations for the timely treatment of hip fractures.
In patients receiving DAPT who require noncardiac surgery, the risk of thrombosis must be balanced against the risk of bleeding. Although many studies have explored the value of bridging antiplatelet therapy in patients receiving DAPT who require noncardiac surgery, most were focused on general surgery cases,[16] while orthopedic cases have rarely been investigated. However, studies have shown that patients receiving DAPT who undergo spinal surgery are at high risk of developing bleeding complications.[11,20] Steele et al[21] summarized the literature on early orthopedic surgery in patients receiving DAPT and concluded that clopidogrel therapy should be continued when possible during the perioperative period, depending on the degree of risk of severe bleeding. According to the 2012 ACCP guidelines,[7] DAPT should be continued during the perioperative period in patients requiring surgical treatment within 6 weeks after bare metal stent implantation or within 6 months after drug-eluting stent deployment. One study reported that nondiscontinuation of aspirin during spinal surgery after PCI did not increase perioperative bleeding.[22] Furthermore, another study reported that heparin was ineffective as a replacement for DAPT[23]; thus, it was suggested that aspirin should be continued for life after PCI and should not be discontinued during the perioperative period of joint replacement.[23]
The current study showed that the volumes of intraoperative hemorrhage, total intraoperative and postoperative hemorrhage, and total perioperative blood loss (calculated based on the change in hemoglobin level) did not significantly differ between patients who continued DAPT or received aspirin alone throughout the perioperative period versus patients who switched to low-molecular-weight heparin therapy for 5 to 7 days before orthopedic surgery. This suggests that the amount of bleeding during orthopedic surgery is not increased by switching from antiplatelet therapy to low-molecular-weight heparin versus the continued administration of clopidogrel combined with aspirin or aspirin alone. Our findings are similar to the results of a previous study.[24]
In our current series, all five patients who developed ACS postoperatively did not receive antiplatelet therapy soon after orthopedic surgery; however, ACS was alleviated after the immediate administration of low-molecular-weight heparin and antiplatelet therapy or intravenous nitroglycerin infusion. One death occurred on the night of orthopedic surgery. In this patient, DAPT was discontinued 5 days after coronary stenting, and 0.6 mL of Fraxiparine was injected subcutaneously every 12 h for 6 days before the orthopedic surgery; no loading dose of DAPT was administered preoperatively.[12] Nine hours postoperatively, the patient developed sudden myocardial infarction and cardiac arrest, and died after failed rescue and resuscitation efforts. DAPT discontinuation should have been contraindicated in this patient. In our series, the incidence of serious adverse cardiac events was 9.1% (6/66), and the risk of serious adverse cardiac events increased when antiplatelet therapy was discontinued preoperatively or was not resumed in time postoperatively.
The 2014 ESC/ESA guidelines suggest that antiplatelet drugs should be stopped 5 to 7 days before surgery.[12] Antiplatelet drug-related bleeding is mainly managed by platelet transfusion. There is no evidence for the effectiveness of heparin or warfarin as transitional treatment after the discontinuation of DAPT.
Continued DAPT or single antiplatelet treatment (with aspirin) during surgery of the spine or extremities does not increase the total intraoperative and perioperative bleeding volume compared with switching from antiplatelet therapy to low-molecular-weight heparin. However, the discontinuation of antiplatelet therapy increases the risk of serious cardiac complications. Our current study was limited by its small sample size; multicenter studies with larger sample sizes are warranted to further evaluate the balance between the risks of massive bleeding versus cardiovascular events in patients receiving DAPT while undergoing orthopedic surgery.
The authors would like to thank Kelly Zammit, BVSc, from LiwenBianji, Edanz Editing China (www.liwenbianji. cn/ac), for editing the English text of this manuscript.
None.






























