
Copyright © 2021 The Chinese Medical Association, produced by Wolters Kluwer, Inc. under the CC-BY-NC-ND license. This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.
To the Editor: Enthesitis is an inflammation of the iliac attachment of ligaments or tendons, which may be among the first symptoms of spondyloarthritis (SpA) and is a unique characteristic of SpA which can differentiate it from rheumatoid arthritis. In spondyloarthropathies, peripheral enthesitis precedes joint symptoms and is associated with a higher degree of erosive disease. Four methods are available for evaluation of enthesitis, including tenderness, conventional radiography, ultrasonography, and magnetic resonance imaging (MRI). However, over 100 entheses are found in the human body. The aforementioned four methods can detect only local enthesitis. Whole-body MRI (WB-MRI) is a novel approach that allows visualization of the entire body in one examination, but has lower image resolution than conventional MRI.[1] Recent studies have explored the application of WB-MRI. However, real-world data are lacking, and most of them are limited to psoriatic arthritis (PsA). In the present study, the distribution pattern of enthesitis was explored in patients with SpA using WB-MRI in real world set. The result was compared with that of other clinical instruments used to evaluate enthesitis.
This study was approved by the Ethics Committee of the Tianjin First Central Hospital (No. 2020N236KY). A total of 50 patients who fulfilled the recently published Assessment of Spondyloarthritis International Society classification criteria for axial SpA (ax-SpA) were included. The exclusion criteria were as follows: (1) patients with serious primary diseases such as cardiocerebrovascular, digestive, hematopoietic system, liver, and renal disease; (2) athletes or practitioners in the fitness industry; (3) history of fracture, joint surgery, or joint replacement; (4) glucocorticoid use in the last 3 months; and (5) contraindications of MRI (pacemakers and so forth). Data of demographics and clinical data were prospectively collected. All patients underwent WB-MRI. Written consent was obtained from all participants before any procedure.
Clinical enthesitis was evaluated using a modified Maastricht Ankylosing Spondylitis Enthesitis Score (MASES) and Leeds Enthesitis Index (LEI). The clinical enthesitis score is the sum of MASES and LEI scores. As the lateral epicondyle of humerus is not in the scope of MRI scanning, it is impossible to make subsequent comparisons. Therefore, it was not counted.
WB-MRI was performed on a Philips 3T Ingenia unit (Philips Healthcare, Best, Netherlands) using phased-array coils with patients in supine position. The technical MRI parameters are shown in [Supplementary Table 1, http://links.lww.com/CM9/A794]. The following 18 locations were evaluated and subdivided into five regions: region 1 included shoulder—acromioclavicular joint and supra-spinatus tendon; region 2 included anterior chest wall— costosternal joints, sternal synchondrosis, and sternoclavicular joints (SClJs); region 3 included pelvis—iliac crest, anterior superior iliac spin, posterior superior iliac spin, ischial tuberosity, pubic symphysis, greater femoral trochanter, and lesser femoral trochanter; region 4 included knee—medial femoral condyles, lateral femoral condyles, condyles lateralis tibiae, and caput fibulae; and region 5 included foot—proximal insertion of the Achilles tendon and plantar aponeurosis. Thirty-six points were assessed for each patient, and a total of 1080 points were assessed for all participants. All MR images were scored independently by two musculoskeletal radiologists. Enthesitis was diagnosed when a high signal intensity on short TI inversion recovery (STIR) images was obtained with a corresponding signal loss on T1-weighted images within the bone marrow (bone marrow edema [BME]) or the surrounding soft tissue (soft tissue edema). WB-MRI was scored dichotomously.
Reliability analyses included intrareader intraclass correlation coefficients (two-way mixed model, absolute agreement definition). The computer software package (SPSS version 25, SPSS, IL, USA) and the R package (R version 3.5.3) were used to perform all statistical analysis. Data were described using means (mean value and standard deviation) and proportions (percentages, %). For the main analyses, WB-MRI results at the lesion level were handled as dichotomous data (present/absent). The MRI results were compared with the clinical results using the McNemar-Bowker test. A P value < 0.05 indicated a statistically significant difference. The correlation of clinical and MRI outcomes was calculated using the Spearman rho (ρ).
Of the 50 patients included, ten were excluded based on the aforementioned criteria. Another ten patients were used as subjects to train two doctors to diagnose enthesitis. The demographic and clinical characteristics of the 30 patients with ax-SpA included in the final analysis are presented in [Supplementary Table 2, http://links.lww.com/CM9/A794]. The patients had a median age of 34.9 years; 20 patients (64.5%) were men and 63.3% were positive for human leukocyte antigen B27. Among the 30 patients, 20 used biological agents, eight used nonsteroidal anti-inflammatory drugs, and two never received treatment.
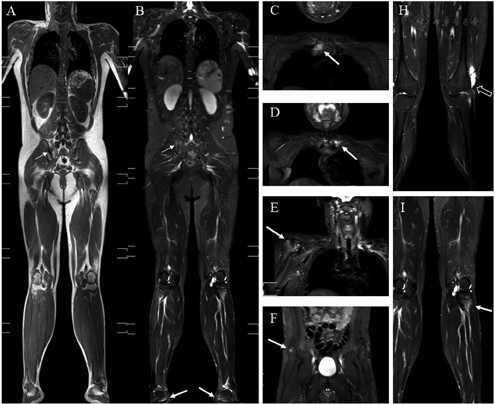
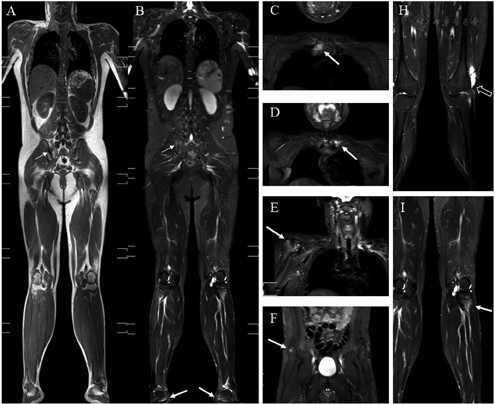
The number and frequency of enthesitis evaluated by WB-MRI and clinically for the individual entheses are shown in [Supplementary Figure 1, http://links.lww.com/CM9/A794]. A total of 450 entheseal sites were evaluated clinically. Clinical enthesitis was observed in 54 of 450 (12%) entheseal sites. The largest proportion of inflammation was detected in the anterior chest wall (n = 24, 44%). The mean clinical enthesitis score was 1.9 ± 2.4 out of 15 possible scoring points. WB-MRI identified enthesitis in 97 of 1020 (9%) entheseal sites. The maximum number of enthesitis cases was detected in the pelvis (27, 28%): including iliac crest one, anterior superior iliac spine three, posterior superior iliac spine 0, ischial tuberosity ten, pubic symphysis four, greater femoral trochanter nine, and lesser femoral trochanter 0. The foot had the least number of enthesitis (12, 12%) cases, whereas the Achilles tendon had eight enthesitis cases. Imaging examples are presented in [Figure 1].
MRI and clinical enthesitis scores were compared to evaluate the proportion of patients with enthesitis among all patients. Overall, enthesitis was detected more commonly by WB-MRI than by clinical assessment. WB-MRI identified enthesitis in 76% of patients (n = 22). However, enthesitis was detected through clinical assessment in only 17 (57%) patients. The detailed results are depicted in [Supplementary Table 3, http://links.lww.com/CM9/A794]. The anterior chest wall (region 1) was affected in 40% of the patients (n = 12) in clinical assessment. The pelvic region was the most frequently affected body region in terms of enthesitis, with 50% affected patients (n = 15), whereas clinical enthesitis in the pelvic region was detected in 20% of patients (n = 6, P < 0.05). WB-MRI enthesitis scores correlated with clinical enthesitis scores (r = 0.45; P < 0.05) but not with Ankylosing Spondylitis Disease Activity Score (ASDAS) scores. Details are provided in [Supplementary Figures 2, http://links.lww.com/CM9/A794 and 3, http://links.lww. com/CM9/A794]. Patients with SpA >5 years had more enthesitis (4.17 ± 3.24; P > 0.05). The ASDAS scores of patients with different courses of disease were similar. Supplementary Table 4, http://links.lww.com/CM9/A794 shows the WB-MRI enthesitis and ASDAS characteristics of patients with different courses of disease. The intrareader reproducibility of WB-MRI assessments was analyzed and the scores of the intrareader ICC for the total number of entheses with enthesitis on WB-MRI (WB-MRI enthesitis score) was 0.91.
In the present study, WB-MRI was used to detect enthesitis in patients with ax-SpA and also to explore the distribution pattern of enthesitis. This was a completely real-world study that reflected the true burden level of enthesitis in patients with ax-SpA, and pelvis and anterior chest wall were the two areas most likely to be affected. Enthesitis of SClJs had the highest proportion. Enthesitis was much less common in the lower extremities, especially in the foot.
Theoretically, MRI could detect more enthesitic lesions compared with the clinical examination. If edema occurs, it can be detected by MRI, while at this time, the patients may be asymptomatic. A possible explanation for the discrepancy between clinical and WB-MRI findings was subclinical inflammation in patients with SpA. This hypothesis was supported by increased radioisotope uptake in the SClJs and manubriosternal joint in 54% of 50 patients with PsA, as opposed to a clinical SClJ involvement in 13%.[2] Another possible reason why MRI detected more enthesitis in the pelvic was that more sites were detected by WB-MRI than by clinical examination, and enthesitis in these sites was likely to be associated with back and hip pain. However, these pains may not be considered as enthesitis, and deep enthesis cannot be detected by tenderness. No correlation existed between WB-MRI enthesitis and ASDAS score. Furthermore, it was speculated that ASDAS could not really reflect the burden of enthesitis in patients. Poggenborg et al[3] found that no significant correlations between peripheral WB-MRI scores and patient characteristics or clinical measures of disease activity were found. However, they found that WB-MRI spinal BME and spinal fat infiltration correlated with the metrology index Bath Ankylosing Spondylitis Metrology Index. Zhao et al[4] concluded that the combination of STIR and DWI would play significant roles in assessing the disease activity, Therefore, it is necessary to further explore the enthesitis and functional MRI results.
The intrareader ICC for the total number of enthesitis on WB-MRI (WB-MRI score) was 0.9 in the present study. This may be improved by increasing the acquisition times. Before reading the image independently, the Outcome Measures in Rheumatology Clinical Trials scoring system was referred to for training.[5] Regarding the research methods, some limitations need to be acknowledged. As long as the water in tissues increases, it can show a high signal in T2-weighted images, irrespective of the cause of the increase. In addition, it is sometimes not easy to distinguish entheseal structure because of the lack of spatial resolution. The scanning strategy needs to be further improved, especially to improve the image quality without increasing the scanning time too much.
Enthesitis affects the quality of life. The existence and distribution of enthesitis may have an impact on the treatment strategy. This study showed that WB-MRI could be a one-stop evaluation of peripheral enthesitis in patients with SpA. WB-MRI might be an up-and-coming tool for the overall assessment of disease activity and injury of PsA and SpA.
None.





























