
Copyright © 2022 The Chinese Medical Association, produced by Wolters Kluwer, Inc. under the CC-BY-NC-ND license. This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.
To the Editor: Cardiac resynchronization therapy (CRT) is an effective treatment for advanced chronic heart failure (HF) patients with reduced ejection fraction. Despite its beneficial effects on cardiac function, traditional biventricular epicardial pacing (BiVP-epi) could not reduce ventricular arrhythmias (VAs) burden in all HF patients.[1] The increase in the dispersion of ventricular repolarization (DVR) after BiVP-epi in non-responders may play a role.[2] Recently, left bundle branch area pacing (LBBAP) has been reported as a feasible option for CRT delivery, while little is known about its influence on DVR. This retrospective study aimed to thoroughly evaluate the changes of DVR after LBBAP in HF patients and compare the repolarization features between LBBAP and BiVP-epi.
HF patients who had undergone successful LBBAP or BiVP-epi from January 2016 to July 2021 were consecutively enrolled. The inclusion criteria were as follows: (1) New York Heart Association functional class II–IV despite optimal guideline-based medications for at least 3 months; (2) left ventricular ejection fraction ≤50%; (3) indications for CRT implantation and/or ventricular pacing; (4) QRS duration (QRSd) ≥130 ms. Postoperative 12-lead electrocardiogram (ECGs) under intrinsic and ventricular-paced rhythm within 24 h were recorded for each patient. Heart rate, QRSd, QT interval, QTc interval, Tpeak-Tend (TpTe), and TpTe/QT were measured in all 12 leads for three beats during sinus rhythm and for five beats during atrial fibrillation, and the averages were taken. To be noted, post-implant TpTe was the primary outcome parameter of the study while the others were secondary outcome parameters, since TpTe was the more commonly used and accurate ECG metric reflecting DVR. The study was approved by the Ethics Committee (No. 2011-366) and obeyed the Declaration of Helsinki. All patients signed an informed written consent form.
A total of 109 HF patients were included in the study, with 49 patients in LBBAP group and 60 in BiVP-epi group [Supplementary Table 1, http://links.lww.com/CM9/B255]. After LBBAP, the repolarization parameters were statistically significantly decreased in comparison with baseline: QTc (446.85 ± 38.56 vs. 477.07 ± 46.27, 95% confidence interval [CI] [-46.19, -14.25] ms, P < 0.001), TpTe (83.60 [74.85, 93.79] vs. 108.17 [95.71, 116.07], 95% CI [-25.60, -16.47] ms, P < 0.001), and TpTe/QT (0.20 [0.19, 0.22] vs. 0.23 [0.21, 0.24], 95% CI [-0.033,-0.019], P < 0.001) [Figure 1]. Besides, there was no statistically significant difference in baseline repolarization parameters between LBBAP and BiVP-epi groups, while LBBAP group showed shorter QTc (446.85 ± 38.56 vs. 480.47 ± 34.69, 95% CI [-47.55, -19.70] ms, P < 0.001), TpTe (84.39 ± 14.12 vs. 113.20 ± 15.68, 95% CI [-34.54, -23.09] ms, P < 0.001), and TpTe/QT (0.20 ± 0.02 vs. 0.25 ± 0.03, 95% CI [-0.06, -0.04], P < 0.001) than BiVP-epi group under paced rhythm [Figure 1]. Of note, multiple linear regression was used to eliminate the potential confounding effects of baseline imbalance between groups and the results showed CRT delivery method (P < 0.001) and the application of amiodarone (P= 0.03) were independently related to repolarization parameters [Supplementary Table 2, http://links.lww.com/CM9/B255]. The effects of different optimization methods on repolarization were also assessed [Supplementary Figures 1–3, http://links.lww.com/CM9/B255]. Repolarization parameters showed no change after AV optimization. LBBAP-optimized CRT (LOT-CRT) statistically significantly increased TpTe (95.58 ± 15.86 vs. 77.84 ± 17.51, 95% CI [7.70, 27.79] ms, P = 0.003) and TpTe/QT (0.23 ± 0.02 vs. 0.19 ± 0.02, 95% CI [0.02, 0.06], P= 0.001) in comparison with LBBAP only. Besides, the addition of right ventricular pacing (RVP) to LBBAP statistically significantly increased TpTe (91.57 ± 12.45 vs. 86.38 ± 12.29, 95% CI [0.49, 9.88] ms, P = 0.03) and TpTe/QT (0.21 ± 0.02 vs. 0.20 ± 0.02, 95% CI [0.001, 0.02], P= 0.03).
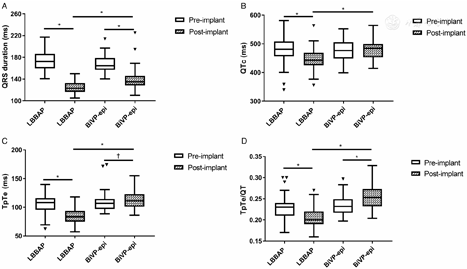
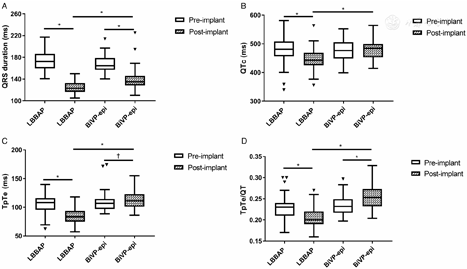
Mitigating the adverse effects of traditional BiVP-epi on DVR is expected to reduce the risks of VAs and even sudden cardiac death (SCD) in CRT patients. One study with merely 13 patients with left bundle branch block (LBBB) induced cardiomyopathy found that LBBAP decreased the QTc, TpTe, and TpTe/QTc,[3] preliminarily indicating the beneficial effect of LBBAP on DVR. The results of the current study further verified the effect in a broader range of HF patients. In addition, the comparison of LBBAP and BiVP-epi on DVR was performed in the current study, and postoperative DVR were statistically significantly lower in LBBAP patients. Since post-implant repolarization parameters have been identified as the independent predictors of appropriate implantable cardiac defibrillator therapy in CRT patients,[2] the better repolarization stability in LBBAP group than BiVP-epi group may suggest lower VAs and low SCD risks in the former group. Yet large, randomized and long-term-follow-up trials are needed to confirm this. Besides, amiodarone was also identified as a significant factor influencing DVR, consistent with its pharmacological nature and previous studies.[4]
In addition, the study found that CRT optimization in pursuit of the narrowest QRSd influenced repolarization in different ways. AV optimization and RVP are both common ways to diminish right bundle branch delay during LBBAP, and the latter was usually used in patients with AV block or atrial fibrillation. DVR showed no change after AV optimization, while the addition of RVP statistically significantly increased DVR. The RV leads were mainly positioned at the apex or the lower septum in our population (mostly the defibrillation leads), thus activation from the cardiac apex to the base reversed the normal electrical propagation and DVR elevation. The addition of epicardial pacing to LBBAP (LOT-CRT) was able to further reduce left ventricular dyssynchrony in LBBB patients.[5] However, DVR was also statistically significantly increased after LOT-CRT due to the reversal electrical propagation from epicardium to endocardium like BiVP-epi. According to these results, it may be more prudent to weigh the risk of DVR deterioration against the benefit of better depolarization synchrony concerning CRT optimization, especially for those with high SCD risks.
In conclusion, LBBAP provided better repolarization status immediately after the implantation than BiVP-epi, and whether the incidence of VAs and/or SCD was lower in the former group remains to be further studied. Besides, the optimization approaches of LBBAP showed various influences on these parameters. The current study provided a reference for HF patients with high SCD risks to choose the optimal way of CRT delivery and optimization.
None.
None.
Li Y, Lu W, Hu Q, Cheng C, Lin J, Zhou Y, Chen R, Dai Y, Chen K, Zhang S. Comparison of immediate changes of repolarization parameters after left bundle branch area pacing and traditional biventricular pacing in heart failure patients. Chin Med J 2023;136:868–870. doi: 10.1097/CM9.0000000000002357





























