
Copyright © 2018 by Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Chinese Medical Association
Please do not use or copy the layout and design of the journals without permission.
All articles published represent the opinions of the authors, and do not reflect the official policy of the Chinese Medical Association or the Editorial Board, unless this is clearly specified.
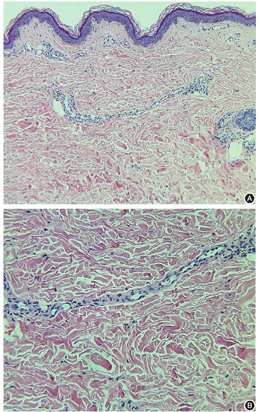
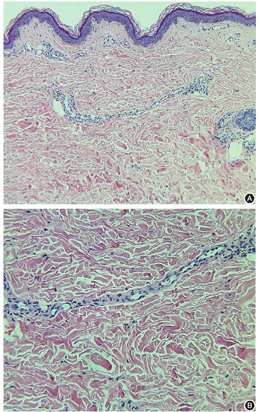
A histopathological examination of skin lesions in mild cases of erythrocyanosis only show lymphocytic infiltration in the upper dermis. In severe cases, dilation of shallow capillaries, endothelial swelling, extravasation of erythrocytes, and occasionally thrombosis in capillaries can also be found. In this case we described here, the epidermis did not show any abnormal features. The dermis showed dilatation of capillaries and perivascular lymphocytic infiltration (Figure 1).
Erythrocyanosis is characterized by the asymptomatic reddish-blue discoloration, usually in the lower extremities. This disease was first reported by Pakers Weber in 1925[1], when he related this " chlorosis in girls and young womem" to wearing tight corsets. It was later named of erythrocyanosis due to the color of its lesion. This disease is relatively rare. Only dozens of cases have been reported at home and abroad since its discovery.
Erythrocyanosis usually presents with reddish-blue discoloration of the skin in the lower half of the leg in girls and young women, especially in the region above the ankle (Figure 2). The color was blanched by pressure. Skin temperature of the legs was normal, but the toes felt cold to the touch.
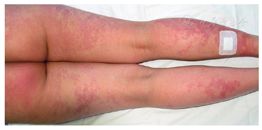
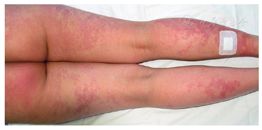
Changes in the skin may also be seen on the buttocks in males. The lesions can be symmetrical or unilateral in erythrocyanosis[2]. The lesions are normally asymptomatic. In more severe cases of erythrocyanosis, sensations of weight and coldness in the leg, intolerable itching, and burning pain, together with the appearance of hypodermal nodules and ulcers, may render the patient unfit for any work[3].
A routine blood test, as well as blood coagulation, blood biochemistry, and blood sedimentation examinations were normal. Anti-PR3 was weakly positive (7.76 RU/ml; normal reference value is < 5 RU/ml). Antinuclear antibody and other auto-antibodies were all negative. The antistreptolysin level was slightly elevated (200 IU/ml; normal reference value is < 116 IU/ml). There were no obvious abnormalities in a B-ultrasound examination of both lower extremities, and arteries and veins.
The cause of erythrocyanosis is not clear, and the disease is exacerbated by cold and usually more prominent during the winter. It is speculated to be the result of the fat layer cutting off heat from blood vessels in the lower extremities[3]. When the outside temperature drops, capillaries of the dermal papillae layer are dilated,leading to reddish-blue discoloration of the skin. In this patient, the severity of the lesion was significantly related to the change of external temperature and body position, suggesting that the disease was related to the vasomotor status of local skin. Additionally, scanty covering of the legs might lead to occurrence of erythrocyanosis because young ladies prefer to wear skirts and thin stockings[1]. Furthermore, sufferers are almost exclusively women, and many cases of erythrocyanosis are first observed at menarche. A slight endocrine disturbance might also be involved in erythrocyanosis[4].
The differential diagnoses of erythrocyanosis include livedo reticularis, erythema induratum, and erythromelalgia. Livedo reticularis is a vasospastic disorder that appears as a violaceous or bluish net-like discoloration surrounding a pale central area of skin. Primary livedo reticularis is a benign condition, which could be exacerbated by cold, tobacco, or emotional upset, whereas the secondary form is a pathological variant seen in association with other vascular diseases or drugs[5]. Erythromelalgia is characterized by recurrent, red, warm extremities accompanied by burning pain, which lasts for minutes to days. Attacks of erythrome-lalgia may be precipitated by warmth, exercise, or limb dependency. Erythema induratum usually presents on the calves of young women. This condition presents as painful violaceous nodules that may be complicated by ulcerations. Some cases represent a manifestation of underlying tuberculosis, which is also known as Bazin disease.
There is no special treatment with a definite effect on erythrocyanosis. Warm clothing and losing weight improves the condition of most patients. In previous case reports, the use of calcium lactate and ultra-violet light baths appeared to be beneficial[1]. In a previous study, 10 severe cases of erythrocyanosis with pain, disability, or total incapacity received operative treatment of bilateral lumbar cord ganglionectomy[3]. Most of these patients had satisfactory results. Because only few studies on erythrocyanosis with small samples have been performed, more high-quality trials with a large sample and longer follow-up are required.
The authors reported no conflicts of interest.





























