
分析3 T MRI三维T2加权快速梯度回波(three-dimensional T2-weighted fast field echo, 3D-T2*-FFE)序列显示胎儿脊柱解剖及椎体畸形的价值。
本研究纳入46例产前超声提示胎儿椎体异常或脊柱部分显示不清的中晚期孕妇,所有胎儿均行脊柱MRI检查,扫描序列包括:3D-T2*-FFE、二维单次激发快速自旋回波(two-dimensional single shot fast spin echo, 2D SSH TSE)和二维平衡式自由稳态进动(two-dimensional balance turbo fast field echo, 2D BTFE)。由两名诊断医师对三个序列获得的脊柱各节段图像质量进行评分,采用非参数检验之Friedman检验比较各序列图像之间评分的差异。对所有病例勾画感兴趣区(region of interest, ROI),并分别计算三个序列颈、胸、腰骶段相应的椎体与椎间盘信号差值比,以评价图像对比度,通过单因素方差分析比较三个序列各节段信号差值比的差异是否有统计学意义。
与2D SSH TSE和2D BTFE序列相比3D-T2*-FFE可以获得更好的胎儿颈椎图像,2D BTFE与3D-T2*-FFE序列在胎儿胸椎及腰骶椎的图像质量均优于2D SSH TSE序列;3D-T2*-FFE和2D BTFE序列的信号差值比高于2D SSH TSE序列,且差异有统计学意义(P<0.05);胎儿胸椎和腰椎在各序列的信号差值比差异无统计学意义(P>0.05)。
3D-T2*-FFE序列对胎儿椎体成像效果较好,能显示更多脊柱解剖细节,其不受胎儿体位影响,且扫描时间较短,临床MRI扫描时可将其作为胎儿脊柱成像的重要补充序列。

本刊刊出的所有论文不代表本刊编委会的观点,除非特别声明
胎儿椎体畸形是目前常见的胎儿畸形之一。先天性椎体畸形可导致出生后脊柱外观异常,部分患者可能合并其他系统异常,如肠闭锁、脑萎缩、尿道下裂等[1]。产前超声是一种成熟的胎儿畸形筛查工具,近年来超声技术的发展使其在胎儿检查中的分辨率得以提高[2]。但是对脊柱的超声评估可能会受到羊水过少、母体肥胖和胎儿体位的限制[3]。胎儿MRI不容易受到这些相关的限制,因此更适用于胎儿脊柱解剖显示和椎体畸形的评估。脊柱异常包括脊柱闭合障碍和神经管缺陷,MRI是明确诊断脊柱异常的重要影像学方法,常规使用的脊柱MRI方案包括二维单次激发快速自旋回波(two-dimensional single shot fast spin echo, 2D SSH TSE)序列和二维平衡式自由稳态进动(two-dimensional balance turbo fast field echo, 2D BTFE)序列[1,4, 5, 6]。与2D MRI序列相比,3D成像序列采用无间距分割的扫描方式,避免了2D成像中信噪比的下降及图像对比度的变化[7, 8]。YANG等[9]认为,三维T2加权快速梯度回波(three-dimensional T2-weighted fast field echo, 3D-T2*-FFE)序列对血流具有更高的敏感性,在显示颈动脉壁方面具有比三维T2可变翻转角快速自旋回波序列更好的黑血效果。XIAO等[10]的研究表明,3D FFE在颈椎脊髓的解剖可视化方面明显优于T2 SSH TSE。目前尚无研究将3D-T2*-FFE序列运用于胎儿椎体成像,本文通过对比胎儿脊柱3D-T2*-FFE、2D SSH TSE和2D BTFE序列的图像质量,评价3D-T2*-FFE序列显示胎儿脊柱解剖及椎体畸形应用中的临床价值。
本研究遵守《赫尔辛基宣言》,并经成都市妇女儿童中心医院伦理委员会批准,免除受试者知情同意,批准文号:科研伦审2022(80)号。对2021年1月至2022年5月在我院放射科接受胎儿脊柱MRI扫描的患者病例进行了回顾性临床研究。纳入标准:(1)妊娠期间超声筛查显示胎儿脊柱异常或脊柱显示不清;(2)孕周≥24周。排除标准:(1)患者行骨盆、腰椎手术(金属伪影);(2)扫描序列不全者;(3)部分患者有明显的胎儿运动,所有序列图像均不能满足诊断要求。46例孕妇资料纳入研究,孕周为24.0~37.4(29.3±3.2)周。
本研究采用Philips Ingenia 3 T MRI,使用16通道相控体部线圈,对母体腹盆腔行大范围冠状位、矢状位及轴位T2加权序列扫描,针对胎儿行2D SSH TSE矢状位、2D BTFE冠矢状位及3D-T2*-FFE矢状位扫描。MRI扫描具体参数见表1。
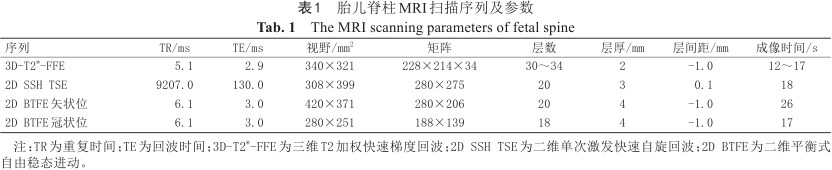
胎儿脊柱MRI扫描序列及参数
The MRI scanning parameters of fetal spine
胎儿脊柱MRI扫描序列及参数
The MRI scanning parameters of fetal spine
| 序列 | TR/ms | TE/ms | 视野/mm2 | 矩阵 | 层数 | 层厚/mm | 层间距/mm | 成像时间/s |
|---|---|---|---|---|---|---|---|---|
| 3D-T2*-FFE | 5.1 | 2.9 | 340×321 | 228×214×34 | 30~34 | 2 | -1.0 | 12~17 |
| 2D SSH TSE | 9207.0 | 130.0 | 308×399 | 280×275 | 20 | 3 | 0.1 | 18 |
| 2D BTFE矢状位 | 6.1 | 3.0 | 420×371 | 280×206 | 20 | 4 | -1.0 | 26 |
| 2D BTFE冠状位 | 6.1 | 3.0 | 280×251 | 188×139 | 18 | 4 | -1.0 | 17 |
注:TR为重复时间;TE为回波时间;3D-T2*-FFE为三维T2加权快速梯度回波;2D SSH TSE为二维单次激发快速自旋回波;2D BTFE为二维平衡式自由稳态进动。
本研究由2名分别具有20年、28年工作经验的副高以上职称且具有胎儿MRI报告审核资质的放射诊断医师对各序列图像进行主观评价,参照VICTORIA等使用的评分标准对三个序列的图像质量进行评分[11]。具体评分标准如下:4分表示解剖结构清晰,组织对比度高,图像质量可达到诊断目的;3分表示解剖结构清晰可见,伪影少,可进行影像学诊断;2分表示图像质量差,伪影明显,可能影响诊断结果;1分表示图像质量差,伪影明显,不能达到诊断目的;0分表示未发现解剖结构。使用非参数Friedman检验比较了序列之间的得分差异。分别于胎儿颈、胸、腰骶段各选取2个连续椎体,在2D SSH TSE序列矢状面手动勾画感兴趣区(region of interest, ROI),并分别复制于3D-T2*-FFE和2D BTFE矢状面的相同位置,ROI位于椎体中央,边缘大致呈矩形,相应区域的平均信号强度(signal intensity, SI)为SIa;勾画并复制两椎体间椎间盘ROI,测量其信号强度SIb。信号差值比*SI的计算公式如下[12]:
SIa表示相邻两个椎体的平均信号值,SIb表示椎间隙的信号值。采用三个序列间的单因素方差分析,比较信号差值比。
使用SPSS 25.0软件进行数据统计处理。对2名诊断医师的图像质量评分进行Kappa一致性检验(Kappa值>0.75表明两者一致性较好,0.40~0.75表明两者一致性中等,<0.40表明两者一致性较差),采用评分平均值进行数据分析,对评分数据行正态性检验分析(K-S检验),采用非参数检验之Friedman检验比较各序列图像之间评分的差异。通过单因素方差分析比较各序列椎体与椎间盘信号对比度差异,并进行组间两两比较,P<0.05为差异有统计学意义。
根据Kappa一致性分析,三个序列的每个脊柱节段的图像质量一致良好,Kappa值>0.75(表2),且各组Kappa一致性分析P<0.001。再取两名医师的评分平均值后进行正态性分析。数据为非正态分布时采用非参数检验的Friedman检验进行比较,三幅序列图像中各脊柱节段的图像质量评分差异有统计学意义(P<0.05)。两两比较显示,3D-T2*-FFE的颈椎图像质量更好,与2D SSH TSE及2D BTFE序列评分差异均有统计学意义(P<0.05);3D-T2*-FFE序列与2D BTFE序列的胸椎和腰骶部图像质量评分差异无统计学意义(P>0.05),2D BTFE和3D-T2*-FFE序列对脊柱各节段的图像质量评分均高于2D SSH TSE序列(P<0.05)。评分结果详见表3。
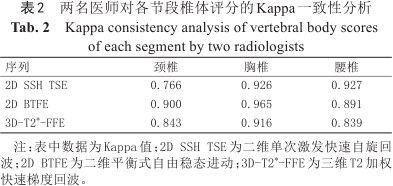
两名医师对各节段椎体评分的Kappa一致性分析
Kappa consistency analysis of vertebral body scores of each segment by two radiologists
两名医师对各节段椎体评分的Kappa一致性分析
Kappa consistency analysis of vertebral body scores of each segment by two radiologists
| 序列 | 颈椎 | 胸椎 | 腰椎 |
|---|---|---|---|
| 2D SSH TSE | 0.766 | 0.926 | 0.927 |
| 2D BTFE | 0.900 | 0.965 | 0.891 |
| 3D-T2*-FFE | 0.843 | 0.916 | 0.839 |
注:表中数据为Kappa值;2D SSH TSE为二维单次激发快速自旋回波;2D BTFE为二维平衡式自由稳态进动;3D-T2*-FFE为三维T2加权快速梯度回波。
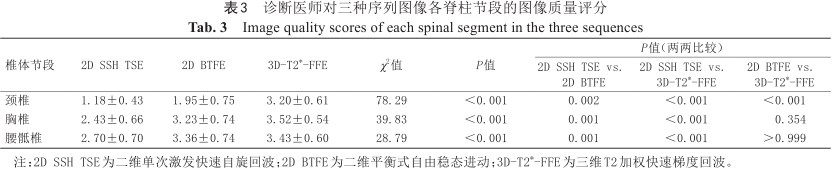
诊断医师对三种序列图像各脊柱节段的图像质量评分
Image quality scores of each spinal segment in the three sequences
诊断医师对三种序列图像各脊柱节段的图像质量评分
Image quality scores of each spinal segment in the three sequences
| 椎体节段 | 2D SSH TSE | 2D BTFE | 3D-T2*-FFE | χ2值 | P值 | P值(两两比较) | ||
|---|---|---|---|---|---|---|---|---|
| 2D SSH TSE vs. 2D BTFE | 2D SSH TSE vs. 3D-T2*-FFE | 2D BTFE vs. 3D-T2*-FFE | ||||||
| 颈椎 | 1.18±0.43 | 1.95±0.75 | 3.20±0.61 | 78.29 | <0.001 | 0.002 | <0.001 | <0.001 |
| 胸椎 | 2.43±0.66 | 3.23±0.74 | 3.52±0.54 | 39.83 | <0.001 | 0.001 | <0.001 | 0.354 |
| 腰骶椎 | 2.70±0.70 | 3.36±0.74 | 3.43±0.60 | 28.79 | <0.001 | 0.001 | <0.001 | >0.999 |
注:2D SSH TSE为二维单次激发快速自旋回波;2D BTFE为二维平衡式自由稳态进动;3D-T2*-FFE为三维T2加权快速梯度回波。
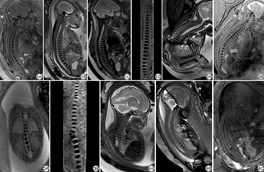
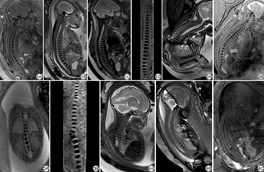
测量每个序列中图像对应ROI的信号值,并计算信号差值比*SI值。所有*SI值均符合正态分布,如表4所示。在胎儿颈椎显示方面,3D-T2*-FFE序列的*SI值高于2D序列,差异有统计学意义(P<0.05);各序列胎儿胸椎和腰骶椎的*SI值差异无统计学意义(P>0.05)。如图1到图4所示:在一些胎龄较大的胎儿图像中,三个序列都可以显示较好的胎儿脊柱图像(图1),但3D序列可通过后处理进行重建,可以提供更多的图像信息;2D BTFE序列受伪影影响较大,3D-T2*-FFE图像质量更佳(图2);图3和图4为胎儿脊柱异常的图像,显示椎体的3D序列明显优于其他两个2D序列。
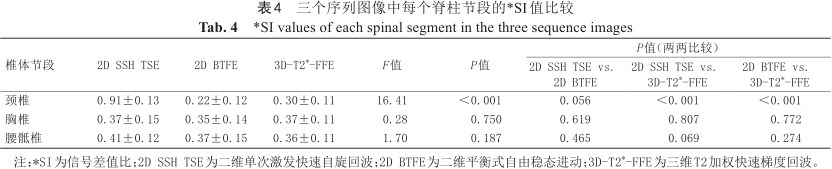
三个序列图像中每个脊柱节段的*SI值比较
*SI values of each spinal segment in the three sequence images
三个序列图像中每个脊柱节段的*SI值比较
*SI values of each spinal segment in the three sequence images
| 椎体节段 | 2D SSH TSE | 2D BTFE | 3D-T2*-FFE | F值 | P值 | P值(两两比较) | ||
|---|---|---|---|---|---|---|---|---|
| 2D SSH TSE vs. 2D BTFE | 2D SSH TSE vs. 3D-T2*-FFE | 2D BTFE vs. 3D-T2*-FFE | ||||||
| 颈椎 | 0.91±0.13 | 0.22±0.12 | 0.30±0.11 | 16.41 | <0.001 | 0.056 | <0.001 | <0.001 |
| 胸椎 | 0.37±0.15 | 0.35±0.14 | 0.37±0.11 | 0.28 | 0.750 | 0.619 | 0.807 | 0.772 |
| 腰骶椎 | 0.41±0.12 | 0.37±0.15 | 0.36±0.11 | 1.70 | 0.187 | 0.465 | 0.069 | 0.274 |
注:*SI为信号差值比;2D SSH TSE为二维单次激发快速自旋回波;2D BTFE为二维平衡式自由稳态进动;3D-T2*-FFE为三维T2加权快速梯度回波。
本研究为国内外首次使用3D-T2*-FFE序列显示胎儿脊柱解剖及椎体畸形。既往的研究多局限于2D BTFE、磁敏感加权成像(susceptibility weighted imaging, SWI)等2D序列进行胎儿脊柱针对性扫描[13, 14]。本研究创新性地使用3D MRI对胎儿脊柱解剖显示及椎体畸形进行评估,研究结果表明3D-T2*-FFE序列对胎儿脊柱的显示效果良好,其扫描时间较短,可通过多种3D图像后处理方法,多方位显示胎儿脊柱图像,有利于胎儿脊柱畸形的早期诊断,具有较高的产前诊断价值。
在胚胎发育过程中,成骨细胞向内迁移,包围脊索,再经软骨化骨而形成椎体,若骨化中心未发育或融合失败,则可导致先天性脊柱侧弯和严重的脊柱畸形[9,15, 16, 17]。产前超声作为胎儿椎体畸形的重要检查方法,广泛应用于临床。但在如孕妇肥胖、肠道气体干扰、胎儿脊柱后位等情况下,超声不能清晰地显示脊柱的椎体,导致诊断困难[18, 19]。随着MRI快速成像序列的发展,2D SSH TSE序列和2D BTFE序列因其良好的图像质量而成为胎儿脊柱成像中最常用的序列[17]。胎儿在宫腔内的位置多变,脊柱轴相对弯曲,椎体结构较小,特别是胎儿的颈椎体积较小。以上两个序列都是2D成像因而导致了微小结构的显示效果相对较差,且不能通过3D后处理来进行多向显示[20, 21]。本研究结果显示,2D SSH TSE序列图像显示椎体边缘不清楚,颈椎表现差,对比度差。2D BTFE序列对椎体显示有良好的影响,但图像伪影可导致局部显示不清,影响图像质量。
由于缺乏氢质子,胎儿椎体的信号较低,与周围组织有明显的对比[22]。3D-T2*-FFE序列采用T2*加权成像,在传统的扫描时间中使用一个较小的翻转角度来实现较高的空间分辨率[23]。T2*-FFE序列优化了序列参数,改善了骨与周围软组织的对比[24, 25]。此外,3D成像序列采用无间距分割的扫描模式,避免了2D成像中信噪比的降低和图像对比度的变化,附加的信息收集使3D成像具有更高的空间分辨率和信噪比[26]。据报道,最常见的产前异常是胸椎(75.4%),其次是腰椎(60.0%)[27]。笔者推测,颈椎先天性椎体畸形的发生率相对较低,椎体体积较小,且对胎儿体位的影响较大,是导致颈椎畸形检出率较低的原因。有研究指出先天性脊柱侧凸与Klippel-Fiel综合征相关,脊柱检查应集中在颈部[28, 29]。在本研究中,主观图像质量评分分析显示,3D-T2*-FFE具有良好的颈椎图像质量,与2D SSH TSE和2D BTFE序列评分差异具有统计学意义。根据客观信号差值比*SI的计算和分析,2D BTFE和3D-T2*-FFE序列的对比优于2D SSH TSE序列,所以3D-T2*-FFE显示胎儿颈椎结构具有较高的诊断价值。
在MRI扫描过程中,胎儿的运动容易产生运动伪影,因此缩短扫描时间是减少运动对图像质量影响的关键。3D-T2*-FFE序列的扫描时间较短,单次扫描时间为12~17 s,可减少胎儿运动产生的运动伪影。另外,本扫描要求孕妇在扫描过程中屏住呼吸,防止呼吸产生的运动伪影,可以进一步提高图像质量,在短时间内提供良好的椎体图像信息。胎儿在子宫腔内的位置是可变的,部分胎儿脊柱轴是弯曲的,3D图像允许评估脊柱的完整解剖,这在2D成像中常常难以实现[30]。传统的2D序列图像可能只显示椎体的边缘部分,导致图像质量较差。通过多平面重建和曲线平面重建等后处理,3D-T2*-FFE可以多方位显示胎儿脊柱图像[31]。CAI等[32]报道了SWI对胎儿脊柱畸形具有良好的诊断价值,因为它提供了骨组织和软组织之间的高对比度。值得注意的是,SWI是一个2D序列,它也有2D序列如2D SSH TSE和2D BTFE的缺点。此外,该研究中的SWI序列要求进行两次屏气,每个周期为13 s,这对被检查的孕妇来说相对难以完成,因此可以认为3D-T2*-FFE序列在胎儿脊柱扫描中更为便利且具有优势。
本研究存在以下局限性:样本量较小;对疑似椎体畸形病例无产后图像资料用以对比验证;仅评估胎儿各节段椎体的影像学检查,未评估脊膜膨出等其他脊柱畸形。此外,部分病例因胎儿运动明显未纳入本研究。因此将进一步增加样本量和出生后发育的长期随访。
总之,3D-T2*-FFE序列对胎儿脊柱解剖结构的显示及胎儿椎体畸形诊断具有一定的临床价值,尤其对胎儿颈椎显示效果较好,且能通过3D后处理提供更多的图像信息,可作为临床应用中的重要补充序列。
何双, 雷强, 王芳, 等. 3 T MRI三维T2加权快速梯度回波序列显示胎儿脊柱解剖及椎体畸形的评价[J]. 磁共振成像, 2023, 14(3): 111-116.
HE S, LEI Q, WANG F, et al. Evaluation of fetal spinal anatomy and vertebral deformity with 3 T magnetic resonance three-dimensional T2-weighted fast field echo sequence[J]. Chin J Magn Reson Imaging, 2023, 14(3): 111-116.
全体作者均声明无利益冲突。



























