
版权归中华医学会所有。
未经授权,不得转载、摘编本刊文章,不得使用本刊的版式设计。
除非特别声明,本刊刊出的所有文章不代表中华医学会和本刊编委会的观点。
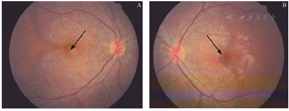
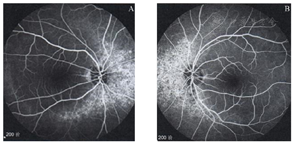
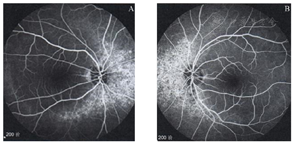
患者,女,18岁,因"右眼视力下降数月"于2015年5月24日来院就诊。患者自觉右眼颞侧视物遮挡,不伴其余眼部及全身不适,否认夜盲史。无外伤史、眼病和全身病史,否认家族中类似情况者。眼部检查:右眼裸眼视力(UCVA)0.16,矫正无提高;左眼UCVA 1.0。眼压正常,双眼眼前段未见明显异常,右眼瞳孔相对性瞳孔传入障碍(Relative afferent pupillary defect,RAPD)阴性。眼底检查见双眼视盘界清,色淡红,后极部大片地图状萎缩灶,其内透见脉络膜大血管,伴色素沉着,右眼病灶累及黄斑中心凹(见图1)。辅助检查:Octopus视野检查见双眼颞侧视野缺损,大致以中线为界(见图2)。双眼光学相干断层扫描(OCT)见双眼视网膜神经纤维层(Retinal nerve fiber layer,RNFL)厚度正常,左眼黄斑中心凹鼻侧视网膜光感受器细胞内外节连接(Inner/Outer segment of photoreceptor,IS/OS)和视网膜色素上皮(Retinal pigment epithelium,RPE)层结构紊乱消失,中心凹厚度180 μm;右眼黄斑中心凹变薄(厚度51 μm),光感受器细胞内外节连接和RPE层结构消失(见图3)。图形视觉诱发电位(Pattern-visual evoked potential,P-VEP)显示右眼无典型P-VEP波形出现,左眼大方格刺激P100波潜伏期延迟,小方格刺激P100波潜伏期和振幅正常。眼底荧光素血管造影(FFA)见早期可见双眼围绕视盘的大片地图状脉络膜萎缩性低荧光区,其内透见脉络膜大血管,造影后期萎缩灶内见大量斑片状荧光着色,夹杂色素性遮蔽荧光(见图4),左眼黄斑中心凹无灌注区轻度损害(见图4A),右眼黄斑中心凹无灌注区损害(见图4B);双眼视盘荧光正常。吲哚菁绿血管造影(Indocyanine angiography,ICGA)见双眼大致以视盘为中心的脉络膜毛细血管稀疏及减少(见图4C-F)。头颅磁共振成像(MRI)检查未见明显异常。诊断:双眼陈旧性脉络膜视网膜病变。
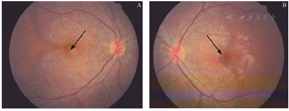
双眼后极部大片地图状萎缩灶,萎缩灶内透见脉络膜大血管,伴色素沉着。A:右眼,病灶已累及黄斑中心凹(见箭头);B:左眼,病灶尚未累及黄斑中心凹(见箭头)
There are large map-like atrophy areas at the posterior pole, with exposed, large choroidal vessels and pigmentation in the fundus of both eyes. A: The macular fovea is involved in the right eye (arrow). B: The fovea is not involved in the left eye (arrow).
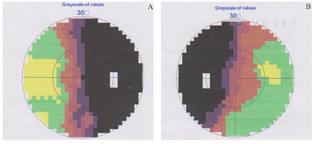
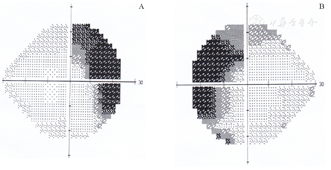
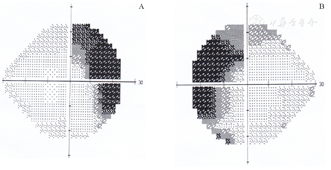
双眼颞侧视野缺损,大致以中线为界。A:右眼;B:左眼
Temporal visual field defect of both eyes, roughly bounded by the midline. A: Left eye. B: Right eye.


A:右眼黄斑中心凹厚度仅51 μm,视网膜光感受器细胞层和RPE层结构消失;B:左眼黄斑中心凹鼻侧、视网膜光感受器细胞层和RPE层结构紊乱、部分消失,中心凹厚度180 μm
A: Similar changes are observed in the macular fovea of the right eye, with a foveal thickness of 51 μm. B: The thickness of the macular fovea of the left eye is 180 μm, and the structure of the retinal photoreceptors and RPE layers is disrupted.


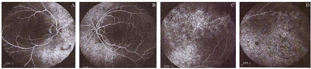
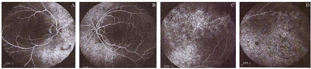
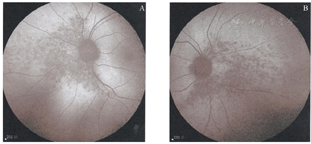
双眼造影后期萎缩灶内见大量斑片状荧光着色,夹杂色素性遮蔽荧光。A:右眼,黄斑中心凹无灌注区损害(见箭头);B:左眼,黄斑中心凹无灌注区轻度损害(见箭头);C、E:右眼ICGA可见以视盘为中心的脉络膜毛细血管稀疏及减少(见箭头);D、F:左眼ICGA可见以视盘为中心的脉络膜毛细血管稀疏及减少(见箭头)
Extensive and patchy fluorescence is mixed with hypofluorescence found in the atrophiedfoci in the late phase of angiography. A: The macula lutea of the right eye is observed with the foveal avascular zone (arrow). B: A mildly damaged foveal avascular zone is revealed in the macula lutea of the left eye (arrow). C, E: ICGA of the right eye reveals an area of a sparse and reduced number of choroidal capillary vessels with the optic disc at the center in both eyes, and the areas in the eye are basically symmetrical (arrow). D, F: ICGA of the left eye reveals an area of a sparse and reduced number of choroidal capillary vessels with the optic disc at the center in both eyes, and the areas in the eyes are basically symmetrical (arrow).
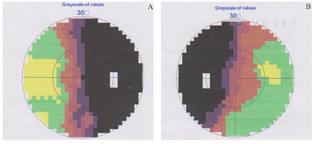
患者,女,45岁,因"双眼视野有遮挡感"于2015年9月3日来院就诊。患者自觉右眼颞侧视物遮挡,不伴其余眼部及全身不适,否认夜盲史。无外伤史、眼病和全身病史,否认家族中类似情况者。眼部检查:右眼UCVA 1.0,左眼UCVA 0.9,均矫正无提高,眼压正常,眼前段未见明显异常。眼底检查见双眼玻璃体清,视盘界清色红润,后极部视网膜未见异常。双眼鼻侧视网膜颜色稍青灰,鼻侧、鼻下方可见骨细胞样色素沉着,双眼病灶对称性分布(见图5)。辅助检查:Octopus视野检查示双眼颞侧视野缺损,部分累及鼻侧(见图6)。眼底自发荧光(Fundus autofluorescence,FAF)检查显示双眼鼻侧病灶为低荧光。FFA示双眼鼻侧高荧光(与自发荧光相对应部位),晚期无明显渗漏(见图7)。电生理检查见暗适应0.1视网膜电图(Electroretinogram,ERG)提示双眼b波振幅重度降低,暗适应3.0ERG提示双眼a、b波振幅重度降低;暗适应3.0震荡电位(Oscillatory potentials,OPs)提示双眼多个子波振幅值重度降低;明适应ERG提示轻中度异常;P-VEP正常。诊断:扇形视网膜色素变性。


双眼眼底后极部未见异常。双眼散瞳下眼底照相检查可见视网膜骨细胞样色素沉着和血管纤细,双眼病灶对称性分布(见箭头)。A:右眼;B:左眼
Nothing remarkable at the posterior poles of both eyes. Bone spicule-like intraretinal pigmentation and vascular attenuation in the nasal and inferonasal retina are seen in both eyes. The retinal disease in both eyes is symmetric (arrows). A: Right eye. B: Left eye.
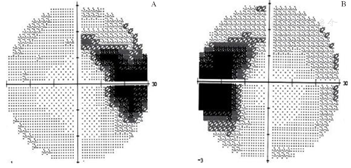
双眼颞侧视野缺损,部分累及鼻侧。A:右眼;B:左眼
Temporal visual field defect in both eyes, some of which involve the nasal side. A: Right eye. B: Left eye.
A:右眼视盘鼻侧高荧光,晚期没有明显渗漏;B:左眼视盘鼻侧高荧光,晚期没有明显渗漏;C:右眼斑片状荧光提示RPE缺损;D:左眼斑片状荧光提示RPE缺损
A: Hyperfluorescence is observed in the nasal retina, and no significant leakage at the late phase in the right eye. B: Similar changes are observed in the left eye. C: Patchy fluorescence reveals RPE defects in the right eye. D: Patchy fluorescence reveals RPE defects in the left eye.
患者,女,69岁,因"发现双眼外侧视野遮挡半年"于2014年3月2日来院就诊。患者自觉右眼颞侧视物遮挡,双眼视力轻度下降,不伴其余眼部及全身不适,否认夜盲史。无外伤史、眼病和全身病史,否认家族中类似情况者。眼部检查:右眼UCVA 0.6,左眼UCVA 0.5,均矫正无提高,眼压正常,双眼眼前段未见明显异常,眼底见双眼视盘边界清,色淡红,后极部视网膜未见明显异常。辅助检查:视野检查显示双眼颞侧视野缺损(见图8)。散瞳后眼底检查见双眼视网膜鼻侧、鼻下方可见骨细胞样色素沉着,局部视网膜血管变细,双眼病灶呈对称性分布。诊断:扇形视网膜色素变性。
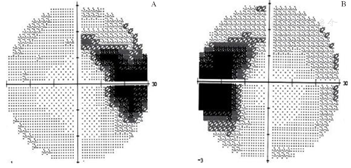
A:右眼颞侧视野缺损;B:左眼颞侧视野缺损
A: Temporal visual field defect of right eye. B: Temporal visual field defect of left eye.
患者,女,45岁,因"双眼闪光感7年余,偶有视物变形"于2018年12月6日来院就诊。患者自觉右眼颞侧视物遮挡,不伴其余眼部及全身不适,否认夜盲史。无外伤史、既往眼病和全身病史,否认家族病史。眼部检查:右眼UCVA 0.8,最佳矫正视力(BCVA)1.0,左眼UCVA 1.0,眼压正常,眼前段未见明显异常。眼底检查见双眼玻璃体清,视盘界清色红润,后极部视网膜未见明显异常。Humphrey视野检查示双眼生理盲点与暗点相连(见图9)。OCT见鼻侧周边病灶部位视网膜和脉络膜结构紊乱,RPE层不连续(见图10)。FAF见双眼鼻侧病灶为低荧光(见图11)。FFA见双眼鼻侧高荧光(与自发荧光相对应部位),斑片状RPE性透见荧光(见图12)。电生理检查见暗适应0.1ERG提示双眼b波振幅重度降低,暗适应3.0 ERG提示双眼a、b波振幅重度降低;暗适应3.0震荡电位提示双眼多个子波振幅值重度降低。明适应ERG轻中度异常。P-VEP正常。诊断:扇形视网膜色素变性。
A:右眼颞侧视野缺损;B:左眼颞侧视野缺损
A: Temporal visual field defect of right eye. B: Temporal visual field defect of left eye.
A:右眼视盘鼻侧视网膜光感受器细胞层和RPE层结构紊乱、部分消失;B:左眼视盘鼻侧视网膜光感受器细胞层和RPE层结构紊乱、部分消失
A: Structural distortion and even disappearance in the photoreceptor and RPE layers can be observed in the nasal retina of the right optic disc. B: Structural distortion and even disappearance in the photoreceptor and RPE layers can be observed in the nasal retina of the left optic disc.
A:右眼鼻侧病灶为低荧光;B:左眼鼻侧病灶为低荧光
A: Nasal lesions in right eye arelow in fluorescence. B: Nasal lesions in left eye are low in fluorescence.
双眼示鼻侧高荧光(与自发荧光相对应部位),斑片状荧光提示RPE缺损。A:右眼;B:左眼
Both eyes show hyperfluorescence on the nasal side (corresponding to the autofluorescence), and patchy fluorescence reveals RPE defects. A: Right eye. B: Left eye. FFA, fundus fluorescene angiography; RPE, retinal pigment epithelium.
以上4例患者视野均表现为双眼颞侧对称性的损害,而最终诊断分别是陈旧性视网膜脉络膜炎和扇形视网膜色素变性。由于视野表现特殊、眼底病灶隐匿、病变进展缓慢等原因,很容易被误诊和漏诊。可能造成双颞侧视野缺损的病因包括:①眼部病变:如青光眼、缺血性视神经病变、脊髓结核性视神经萎缩;②颅脑病变:如创伤性交叉综合征、鞍区脑膜瘤、空蝶鞍综合征、鞍区黄色肉芽肿、前颅底脑膜瘤、颅咽管瘤、垂体瘤、基底性脑膨出、垂体结核瘤、视交叉海绵状血管瘤、囊肿、脓肿、动脉瘤;③其他:多发性硬化、神经梅毒等。因此,双颞侧偏盲的病因相对多而复杂,但本组4例患者和我们最常想到的视交叉受损不同,均是由视网膜病变所致[1,2,3,4,5,6,7,8,9,10,11],部分病例曾被误认为是双颞侧偏盲[11]。只有视交叉中来自交叉的双侧视网膜鼻侧纤维受损所致的视野缺损才被称为"双颞侧偏盲",可以对称出现,表现为典型的双颞侧偏盲;也可以不对称出现。本研究病例主要是因为双眼鼻侧视网膜病变所致双颞侧视野缺损,因此不属于双颞侧偏盲。病例1患者为年轻女性,右眼视力下降数月,瞳孔RAPD阴性,且无伴眼球转动痛,不符合球后视神经炎的典型表现。进一步检查后发现双眼视野缺损与视网膜脉络膜萎缩部位存在对应关系,头颅MRI排除了颅脑病变,追问病史,患者自诉起病前有高热、昏沉病史,因此考虑患者的双眼鼻侧视野偏盲是由双眼视网膜脉络膜病变引起的,患者病程较长,随访7年病情静止,因此支持陈旧性视网膜脉络膜病变的诊断,病因可能与全身病毒感染有关。
病例2患者主诉双眼视野遮挡,散瞳后双眼眼底发现鼻侧周边视网膜病灶,骨细胞样色素沉着,双眼病灶对称性分布,不难诊断为视网膜色素变性,首次就诊时未散瞳看眼底,怀疑鞍区病变,外院行头颅MRI检查排除了颅内疾病后考虑视网膜病变。病例3患者双眼外侧视野遮挡半年,散瞳后双眼眼底发现周边视网膜病灶,见骨细胞样色素沉着呈对称性分布,即诊断为双眼扇形视网膜色素变性。病例4主诉双眼闪光感7年余,偶有视物变形,患者7年前即发现双眼颞侧视野周边暗点,且与生理盲点相连,7年间病情进展,期间患者曾于当地医院规律复查,均未查出病因,7年后于我院就诊时发现双眼底视盘鼻侧视网膜血管变细,视盘鼻侧视网膜颜色晦暗,随后进一步的检查支持扇形视网膜色素变性的诊断。扇形视网膜色素变性又称象限性视网膜色素变性,通常为常染色体显性遗传,其病变局限于眼底的某一个或2个象限,呈扇形分布或者占半侧眼底,常位于下方2个象限,如只侵犯一个象限,以鼻下方象限常见。两眼发病并且通常对称,一般病情进展缓慢,如本病例4所示,7年间病情缓慢进展。该类患者多无夜盲主诉,供应病变区的视网膜血管变细,视野缺损一般与病变区相对应,电生理检查以暗适应ERG受累较重。病例2、3、4均为较典型的扇形视网膜色素变性,其诊断的关键均在于散瞳仔细检查周边视网膜时,发现了鼻侧周边部视网膜病灶及骨细胞样色素沉着。确诊并不困难,但是由于眼部检查不够仔细全面,根据特殊视野表现极易将病变定位于鞍区,误以为是视交叉受损,因此给患者带来了不必要的心理和经济负担。
以上4例患者的视野均表现为双眼颞侧对称性的损害。对称性的双眼鼻侧视网膜病变少见,多为围绕视盘边缘或视盘附近的视网膜、脉络膜疾病,因该部位局部退行性变、炎症、肿块等病变影响视网膜局部功能导致视野相应的改变,常见的研究报道包括扇形视网膜色素变性、陈旧性视网膜脉络膜炎、匐行性脉络膜炎等[11,12]。对于此类病例出现特殊视野改变,散瞳后进行仔细的眼底检查是诊断疾病的关键。此外即使有明确的视网膜病变解释视野缺损,常规头部的影像学检查仍然是必不可少的,以明确患者是否存在或合并鞍区病变。此外,本研究患者出现对称性眼底损害的原因尚不清楚,还应长期观察。
本研究无任何利益冲突


























