
肾脏囊性疾病是引起儿童肾脏发生囊性改变的主要疾病,是指由不同原因引起肾脏发生单个或多个含液体囊腔的一系列先天性或获得性疾病。随着超声诊断技术的不断发展和广泛应用,超声在反映肾脏囊性病灶的结构特征方面,一定程度上优于CT和磁共振成像,越来越得到儿科医师的认可。现总结分析儿童常见肾脏囊性疾病的超声影像学特点,为临床诊断提供帮助。

版权归中华医学会所有。
未经授权,不得转载、摘编本刊文章,不得使用本刊的版式设计。
除非特别声明,本刊刊出的所有文章不代表中华医学会和本刊编委会的观点。
儿童肾脏囊性疾病是一组由不同原因引起的肾脏出现单个或多个含液体囊腔的疾病。形成囊腔的原因很多,不能简单地将肾脏多囊性疾病归为多囊肾,可分为先天性和获得性,主要包括发育异常、基因突变、液体分泌增加、梗阻等,可以单独存在,也可以与其他疾病共存或表现为综合征[1]。CT和磁共振成像(MRI)对肾脏占位的识别能力优于超声,而在诊断肾脏囊性疾病方面,超声更具优势。有文献报道,超声诊断单纯肾囊肿的可靠性达95%以上,同时在反映囊肿壁、囊内分隔或囊液性质等方面明显优于CT[2]。超声检查无放射性损伤、操作方便、可重复性高,对含液体成分的诊断敏感性、特异性均较高。且儿童腹壁较薄,结合高频超声探头的应用,超声可更清晰地显示肾脏微小囊性结构,已经越来越得到儿科医师的认可,成为易被X线损伤的儿童常规肾脏检查及复查的首选检查方法。现总结儿童常见肾脏囊性疾病的超声影像学特点,为临床诊断提供帮助。
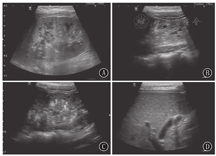
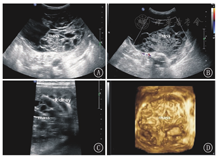
MCDK是婴幼儿肾脏最常见的囊性发育异常性疾病,发病率约为1/3 000[3],是一种非遗传性完全性肾脏发育不良,由于其多囊的超声表现常误诊为多囊肾。因为双侧MCDK患儿不能存活,所以单侧发病多见,患侧肾脏多无功能,同侧输尿管多闭锁或未发育,对侧肾多发育正常,由于对侧健康肾脏代偿性增大,肾功能正常。单侧MCDK患者,临床多无特异性症状和体征,预后良好,一般也不发生癌变,可手术切除[4,5];如果对侧肾脏发育异常,如常合并肾盂输尿管连接部梗阻、重复肾、膀胱输尿管反流等[6],预后则取决对侧肾脏的异常严重程度,如同时伴肾外畸形,则预后不良。MCDK典型的超声影像学特点是患侧肾脏失去正常形态,由数量不等、大小不一的多个薄壁囊肿组成,各囊肿互不相通,囊肿间由于结缔组织增生看不到肾实质或仅有少部分肾实质(图1)。同侧输尿管多不显示。同时要仔细观察对侧肾脏是否发育正常,有助于评估预后。大多数患儿在产前超声检查时发现,出生后的患儿需要超声密切随访观察肾脏发育状况[7],该病可随时间推移而发生退化,最终演变为小瘤样组织。当患儿出现血压增高或患侧肾脏合并巨大囊肿时需手术切除,因此,对MCDK囊肿大小的评估至关重要。本病与重度肾积水不同,一般情况下,重度肾积水内的多个液性囊腔是由明显扩张的肾盂肾盏形成的,彼此连通,囊腔间可见菲薄的肾实质,探查肾盂输尿管连接部具有重要的诊断意义[8]。


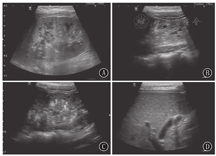
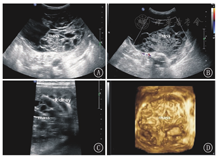
ARPKD是一种儿童最常见的遗传性囊性肾脏疾病[9]。该病存在第6号染色体上的PKDH1基因突变[10],子代个体中1/4发病,而父母双方均无本病表现。肾脏的主要病理学改变为集合管及远端肾小管弥散性扩张,呈放射状排列,从髓质扩展到皮质,部分患者扩张的囊腔内有钙盐沉积或尿酸盐小结晶可见。患儿均出现不同程度的先天性肝脏纤维化。根据发病年龄、肾小管受累数量及肝脏损害程度分为4型:围生期型、新生儿型、婴儿型和少年型。前两型在胎儿或新生儿期就表现为双侧肾脏对称性增大且回声异常,预后较差,通过超声检查可确诊。后两型出生时肝肾病变较轻,无明显临床症状和体征,随着年龄的增长,患儿逐渐出现消化或泌尿系统症状而确诊[11,12]。以往认为肾脏病变程度与肝脏病变程度成反比,年龄越小,肾脏病变越重的患者,肝脏纤维化的程度反而越轻,而有研究认为二者的发展各自独立,并无相关性[13,14]。年龄越小的ARPKD患者肾脏超声影像学特点越典型。胎儿或新生儿患者往往出现双肾对称性明显增大,但并不失去椭圆形的外形,皮髓质分界不清,有时可见外围一圈薄薄的正常肾皮质,严重者肾被膜显示不清晰;低频凸阵探头显示髓质回声增高的典型超声改变,是由于髓质内数量众多的微小囊肿及扩张的小管所产生的声波多重反射形成;线阵高频探头可显示髓质内弥散密集分布的条状或管状微小囊腔结构(扩张的集合管和远端肾小管)或皮髓质散在多发小囊肿,部分患儿囊腔内有钙盐沉积或尿酸盐小结晶形成的成簇成团的点状强回声,为本病的特异性超声表现(图2)。而年龄较大的ARPKD患儿,病变主要以肝胆改变为主、肾脏病变不明显[15],双肾呈轻、中度增大,可能是由于患儿年龄偏大,部分患肾在病程进展中逐渐缩小,因此肾脏增大的患儿较少[9]。有学者使用超声追踪随访ARPKD患者,发现肾脏体积随年龄增大可保持不变,也可逐渐缩小[16]。也有学者认为ARPKD患肾体积的改变与肾功能并无确切相关性[17]。因此,对较大年龄患儿诊断ARPKD,肾脏大小不是诊断的关键,髓质内有无微小囊腔结构及肾实质内有无散在囊肿才是本病主要的诊断依据。怀疑ARPKD的患儿,尤其是对于较大年龄患儿,常规探查肝脏有助于ARPKD的诊断。观察肝内胆管有无扩张,肝叶比例有无改变,肝脏有无纤维化及纤维化的程度等(图2)。一般情况下,肝叶比例改变均表现为左叶增大、右叶缩小[18]。结合临床特点、基因检测结果和超声影像学特点,不难做出ARPKD的诊断。
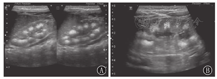
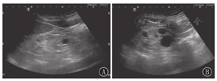
ADPKD是全球发病率最高的单基因遗传性肾病,其发病率为1 /1 000~1 /400,主要是由位于第16号染色体上的PKD1和第4号染色体上的PKD2基因突变引起,有家族史,多于成年后发病,且预后不良,儿童发病少见[10]。ADPKD是一种以器官内囊肿形成为特征的全身性疾病[19],可多器官受累,因此常合并多囊肝、多囊脾、多囊胰等。肾脏的主要病理学改变为肾小管上皮细胞来源的充满液体的囊泡不断形成和扩张,最终与集合管连接不良,尿液排出受阻引起肾小管形成潴留性囊肿,进行性增大,肾脏表面及内部可见大小不等的肉眼可见的囊肿,肾实质残留很少。病变为双侧。患儿年幼时肾脏外形、大小正常或略增大,随着年龄增长,肾内囊肿的大小和数目不断地增大、变多,多数患者40~50岁时肾脏才会出现症状。儿童ADPKD双侧肾脏改变多不典型,超声表现为双肾大小正常或稍大;肾脏的超声表现多数正常或难以断定,肾实质内可见数个囊肿聚集或呈散在分布,囊肿较小、较少,肾实质回声可见;肾盂肾盏均保持正常形态,肾窦未见受压,随着年龄的增长及病情进展,囊肿逐渐增大、增多,囊肿间彼此不相通,囊壁可见成团成簇的强回声点,双肾明显增大,形态失常,表面凹凸不平,肾实质变少(图3)。对于疑似ADPKD患儿,临床应询问家属是否有家族史,综合分析得出诊断。若实际情况需要则应告知患儿要定期复查,随访观察肾内囊肿的发展变化。


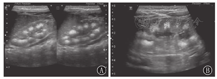
MSK是一种以肾锥体部的集合管弥散性扩张为主要特征的先天性肾髓质囊性病变,其实质是小管扩张,而非真正囊肿性疾病。1939年Lenarduzzi首次对MSK进行了描述[20]。该病无家族史,发病率为1/20 000~1/5 000,可以独立存在,也可以是某个先天综合征的一部分,以肾脏集合管弥散性扩张为特点[21]。但多数患者无症状,实验室检查正常。儿童期起病者少见,临床表现无特异性,多由行腹部超声检查时偶然发现[22,23]。该病双侧发生多见,病变与ARPKD不同,ARPKD随着病情的进展,可同时累及皮髓质,而MSK仅局限于髓质锥体部。肉眼可见肾髓质区多发微小空洞,肾锥体集合管呈线性扇状排列,外观似海绵样,故称海绵肾。由于肾乳头先天性发育异常,其进入肾小盏部位类似括约肌的结构肥厚、收缩,导致乳头管和集合管梗阻而出现囊状扩张、迂曲,产生囊性空腔[24],多数直径为1~3 mm,扩张的囊腔内可充满钙盐,形成砂粒样细小结石。本病超声影像学特点为常累及双侧肾脏,肾脏正常大小或稍大。单个肾锥体呈放射状分布的高回声区,各锥体间呈花瓣样排列,这是由于扩张的集合管囊腔较小,管壁形成大量的反射界面,同时内部伴成簇成团的小结石所致(图4)。肾皮质回声均匀,较正常略薄。本病需与多种原因引起的肾钙质沉着症鉴别。肾钙质沉着症为多种原因引起的肾锥体内钙盐沉积,多见于高血钙症,在原发性肾小管酸中毒、甲状旁腺功能亢进和慢性肾盂肾炎等疾病时最常见,鉴别时需结合临床特点[25]。
2016版世界卫生组织(WHO)肾肿瘤分类将旧版中肾母细胞瘤名下的CPDN与肾母细胞瘤列为并列的亚类,增加了儿童CN这一亚类[26]。两者均无家族史,一般不伴其他异常,临床症状无特异性,通常无症状,幼儿多为腰腹部触及或临床体检时偶然发现包块就诊,其影像学检查及大体标本上也相似,鉴别须行病理镜检。CPDN和CN的主要鉴别依据是前者的间隔内含有胚芽成分和不成熟组织,而后者没有。CPDN 1975年由Brown首次提出,至今国内外报道甚少[27],多发生于2岁以内男童,左肾多于右肾,肿瘤通常较大[28]。CPDN与儿童CN均为多房囊性肿物,局限于同侧肾脏的一部分,与肾组织间仅一层薄膜相隔,未受累肾组织正常。CPDN和CN的超声图像类似,无法鉴别,其共同超声影像学特点多为单侧肾脏受累,肾脏的某一部位可见一单发的含有较多纤细分隔的囊性肿物,多为类圆形或椭圆形,边界清晰,有包膜,囊内均为无回声,囊壁及分隔上均无血流信号,未受累区肾脏组织正常(图5)。
ARCD多见于尿毒症或接受透析的慢性肾衰竭的患者,随着透析时间的延长,该病的发生率逐渐增加[29]。囊肿的形成原因不明,可能与透析导致肾小管基膜改变、上皮增生、间质纤维变性有关。出现ARCD后,肾肿瘤的发生率也会大大增高,增加了肾病患者的危险程度[29]。Dunnill等[30]于1977年首次提出该疾病,并进一步描述了该疾病与肾肿瘤的相关性。一旦出现ARCD,就需要对病变肾脏进行定期超声检查随访,排除肿瘤的可能。该病在儿童中较为少见,其超声影像学特点为患者双侧肾多较小,实质回声增强、皮髓质界限不清,呈弥漫性损伤改变。ARCD以多发为主,也可单发,形态欠规则,囊壁较单纯囊肿厚,且毛糙(图6)。一般情况下,一定时间内随访观察囊肿的大小变化不明显[31]。
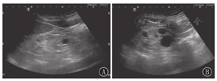
单纯肾囊肿又称为孤立性肾囊肿,好发于成人,儿童罕见[32]。该病囊壁薄而透明,常以单独疾病出现。超声检查可确诊该病,表现为一侧或两侧、单个或多个,孤立于肾皮质或髓质内边缘锐利类圆形透声区,囊腔与肾盂不相通,囊肿外肾组织正常(图7)。该病预后通常较好,一般建议随访观察,当囊肿增大、数目增多压迫肾实质或引起临床症状时可考虑手术治疗[33]。


综上,儿童肾脏囊性疾病在临床上比较常见,实为多种病因、多种表现形式的一组疾病,临床结局也不尽相同。而超声检查能鉴别各肾脏囊性疾病的具体类型,对患儿可能出现的预后给出合理评价及意见。
所有作者均声明不存在利益冲突



























