
Copyright © 2018 by Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Chinese Medical Association
Please do not use or copy the layout and design of the journals without permission.
All articles published represent the opinions of the authors, and do not reflect the official policy of the Chinese Medical Association or the Editorial Board, unless this is clearly specified.
Erythrokeratoderma variabilis is a rare autosomal dominant genodermatosis that usually appears within the first year of life, but may arise later in childhood. EKV was described by Mendes da Costa in 1925[1]. Clinical characteristics of EKV consist of irregularly-shaped, erythematous, scaly patches and hyperkeratotic plaques.
Currently, no standard therapy is available for EKV. Oral vitamin A, systemic retinoids such as isotretinoin and acitretin alone or combined with PUVA therapy have been reported to apply in treatment of EKV. However, it is common that EKV relapses when above therapies are discontinued. Topical emollients and keratolytics such as urea, salicylic acid, propylene glycol, and lactic acid have also been documented for therapy of EKV[2,3,4,5].
Herein, we reported a 3-year-old male child with EKV, who showed a satisfactory response to 10 mg/day acitretin and topical 0.025% tretinoin cream, with almost normalization of lesions within just 2 weeks.
A 3-year-old male child presented to the Hospital for Skin Diseases with generalized, irregularly-shaped, erythematous, scaly patches and hyperkeratotic plaques located on the lower abdomen, inguinal fossa, buttocks, limbs, axillae, and face (Figure 1A-D) since his neonatal age. These erythematous lesions were observed to change in shape and position over time. The lesions were asymptomatic and became worse in summer, while no palmoplantar keratoderma was observed.
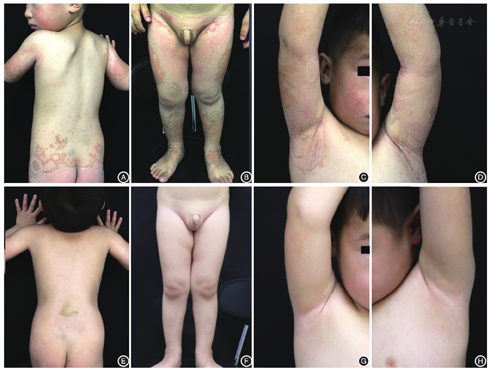
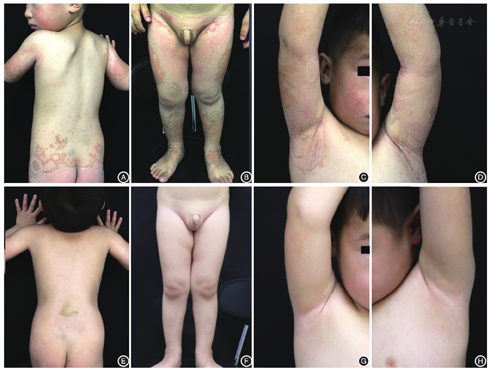
A systemic examination and developmental milestones were normal. Microscopic examination of fungi was negative. Histopathology of a fixed hyperkeratotic plaque showed hyperkeratosis, papillomatosis, acanthosis, and perivascular lymphocytic infiltration in the upper dermis. On the basis of these findings, a diagnosis of EKV was made.
The patient was initially treated with oral acitretin at a dose of 10 mg/day (equivalent to 0.6 mg/kg) and topical 0.025% tretinoin cream per night based on the normal fasting lipid profile and liver function tests. Two weeks later, there was a dramatic response to the treatment, with almost complete remission of the lesions (Figure 1E-H). There were no immediate adverse effects. And then, the use of topical tretinoin cream was stopped, and the dose of acitretin was reduced to 10 mg every other day for one month, and no recurrence of the lesions was found during the following 2 months.
As far as our extensive review of the published work has revealed, successful use of acitretin in treating EKV in children has rarely been reported. Robin et al.[6] reported that a 9-year-old girl with EKV rapidly improved by a 3-week treatment of oral low-dose (15 mg/day, equivalent to 1 mg/kg/d) acitretin. In our case, the lesions of the patient almost disappeared with just 2 weeks treatment of oral acitretin and topical tretinoin.
However, the use of oral retinoids in children remains controversial because of its potential adverse reactions, especially premature epiphyseal closure and growth retardation. Recently, Liang et al[7]. conducted a retrospective investigation of three children, who were afflicted by a severe hyperkeratotic disorder. These children were continuously administrated with 0.2-0.3 mg/kg per day acitretin for longer than 12 years after an initial period at a larger acitretin dose. They found that acitretin monotherapy was an effective treatment for these children, and maintenance doses were well tolerated, with no skeletal or other observable side effects during the study. Despite this finding, baseline radiographic assessment, either by radioisotope bone scanning or selective skeletal survey, is recommended to exclude any skeletal abnormalities related with retinoid therapy.
In this case, the close differential diagnosis includes progressive symmetric erythrokeratoderma (PSEK), pityriasis rubra pilaris (PRP), and nonbullous congenital ichthyosiform erythroderma.
Similar to EKV, PSEK is a rare, autosomal dominant inherited disorder that manifests soon after birth with erythematous, hyperkeratotic plaques. However, its characteristic clinical lesions are symmetrically distributed on the extremities, buttocks, and face, sparing the trunk, which may regress at puberty[8]. PRP may be classified into six types and juvenile types should be excluded in our case. The diagnosis of PRP depends on its distinctive clinical characteristics, such as redorange color follicular papules on the backs of the fingers, sides of the neck, the sandal-like palmoplantar hyperkeratosis,and the sparing islands of normal skin in the midest of the lesions[9]. Nonbullous congenital ichthyosiform erythroderma is an autosomal recessive dermatosis and affected infants are born enclosed in collodion-like membrane. As the membrane is shed, underlying redness and scaling with generalized involvement are apparent. Cicatricial alopecia and nail dystrophy always coexist with the lesions[10] .
The histopathological findings of EKV are nonspecific, with variable degrees of acanthosis and hyperkeratosis of the epidermis, and mild perivascular lymphocytic infiltration in the dermis.
In summary, we reported a 3-year-old boy with EKV, who showed an excellent response to oral acitretin at a dose of 0.6 mg/(kg· day) and topical 0.025% tretinoin cream. The lesions showed almost complete normalization within only two weeks. Our current evidence suggests that comibned treatment of oral acitretin with topical 0.025% tretinoin cream has minimal side effects and good tolerance with a low cost. This treatment might become a satisfactory choice for children with EKV.
The authors reported no conflicts of interest.





























