
Pterygium inversum unguis (PIU) refers to a disorder that distal portion of the nail bed adheres to ventral surface of the nail plate, leading to the absence of the distal groove. This is not a common condition in existing literature, thus its pathogenesis has not been elucidated. The occurrence can be congenital, idiopathic, or secondary. Here we present a case of PIU associated with systemic lupus erythematosus (SLE).
A 33-year-old woman presented with distal nail bed of the bilateral fingers (excluding the thumbs) adheres to the ventral surface of the nail plate, associated with a malar rash, photosensitivity, and arthritis, whose further laboratory examinations confirmed immunologic disorders. All these clinical characteristics and laboratory results point to the diagnosis of PIU secondary to SLE. Treatment of SLE and topical application of tretinoin 0.025% were performed and resulted in the improvement of most discomforts but PIU. There has no aggravation or alleviation of the PIU during a year of follow-up.
Acquired form of PIU is reportedly associated with connective tissue diseases or other conditions, which may be caused by abnormal distal circulation or exposure to certain chemical stimuli. Some therapies may be available, while the most effective strategy is to treat potential disorder. Clinicians should be vigilant to find out the underlying causes of PIU, so as to obtain better therapeutic efficacy.
We observed a rare disorder of PIU associated with SLE. Hence when identifying a patient of PIU, comprehensive evaluations and long-term follow-up are imperative to to detect the development of connective tissus diseases, such as SLE.

Copyright © 2020 Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences, and Chinese Medical Association, published by Wolters Kluwer, Inc.
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NCND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.
Pterygium inversum unguis (PIU), also known as ventral pterygium, is a rare abnormality characterized by adherence of the distal nail bed to the ventral surface of the nail plate, resulting in obliteration of the distal groove. PIU was first described by Caputo and Prandi in 1973 in a woman who developed ventral pterygium on multiple fingers of both hands without definite cause.1 This condition, which have been reported in few cases, can be congenital, idiopathic, or secondary to systemic connective tissue diseases or other. We herein report a case of acquired PIU associated with systemic lupus erythematosus (SLE), which is rare of its kind in the Chinese dermatologic literature.
A 33-year-old woman presented with a 2-year history of multiple telangiectasias in the abdomen of the fingers in May 2018. The telangiectasias were scattered between bright red or purple patches. She was initially treated for frostbite with topical heparin ointment. One month before the current visit, she presented with proximal muscular weakness, a malar rash, photosensitivity, knee and ankle arthritis, and PIU of the fingers. She complained for mild to moderate pain while clipping her fingernails. She was then admitted to our hospital.
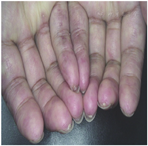
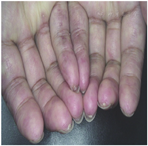
Physical examination of the fingernails (excluding the thumbs) revealed marked subungual keratotic thickening between the distal hyponychium and ventral nail plate. The distal portion of the nail bed was adherent to the ventral surface of the nail plate, obliterating the nail groove (Fig. 1). The patient had no family history of a similar nail abnormality. The laboratory findings were consistent with the diagnosis of SLE (positive for ANA, Ro/SSA, La/SSB, U1-SnRNP antibody, anti-dsDNA, and Smith antibody).
The patient was treated with methylprednisolone (40 mg/day), mycophenolate mofetil (1.0 g twice a day), and hydroxychloroquine (0.2 g twice a day). In addition, her nails were treated by topical application of tretinoin 0.025%. Approximately 2 months after the beginning of treatment, most of the SLE symptoms had disappeared or improved; however, the nail disorder has not been improved. The patient had no adverse or unanticipated reactions and was satisfied with the effect.
Regular follow-up has been undergoing until the time of this writing. The patient continued to use topical agent of tretinoin 0.025% at the sites of pterygium intermittently and attend the clinic regularly. The SLE symptoms were well controlled, while PIU was not significantly aggravated or alleviated. Without obvious discomfort, the patient refused other possible treatment options and gave the informed consent for publishing her case.
We have herein described a case of a 33-year-old woman with a recent diagnosis of SLE, in whom the distal portion of the nail bed of the bilateral fingers (excluding the thumbs) was adherent to the ventral surface of the nail plate, obliterating the groove. The patient in the present case had an acquired form of PIU affecting all of the fingernails (excluding the thumbs) without involvement of the toenails.
Acquired PIU is reportedly associated with connective tissue diseases such as systemic sclerosis2 or other conditions such as stroke, onychophagia, allergic dermatitis, or use of gel polish, and after allogeneic haematopoietic stem cell transplantation.3,4,5,6 Because of the rarity of this condition, its exact origin remains speculative. In order to better recognize the origin and pathology of this infrequent disease, Zaias et al.7 classified it into three categories: congenital aberrant hyponychium, acquired irreversible PIU, acquired reversible extended hyponychium. Acquired form of the disorder may be linked to abnormal distal circulation or exposure to certain chemical stimuli, which leads to destruction of the matrix, reactive hyperkeratosis and thus pterygium formation.4,7 This may explain the pathogenesis of our patient, who could be categorized into acquired irreversible PIU, secondary to SLE.
The management of PIU is not well defined. Different treatments, including topical retinoids, hydroxypropyl chitosana, and electrodissection, can reportedly produce a good response.8,9 The most effective strategy involves treatment of the underlying cause of acquired PIU. In our case, however, the PIU did not improve after 2 months of treatment of SLE and use of topical retinoids. The patient was still undergoing follow-up at the time of this writing.
In conclusion, patients with PIU must be evaluated to rule out associated causes, and these patients require longterm follow-up examinations to detect the development of connective tissue diseases such as SLE.
The authors reported no conflicts of interest.






























