
Acne scars are caused by inflammatory reactions, infections, and improper handling of acne lesions. Such scars have a high incidence and are difficult to treat. There are many methods currently used to treat acne scars, including medications, photoelectric technology, surgery, filling, chemical peeling, traditional Chinese medicine, biotherapy, and microneedle therapy, and many new methods are constantly emerging. However, there are still many issues, such as the lack of high-quality clinical studies, non-uniform treatment methods, and unsatisfactory therapeutic effects. The selection of appropriate methods for the comprehensive treatment of different types of acne scars at different stages in clinical practice remains challenging and is a research topic of great interest. From the perspective of evidence-based medicine, this consensus aims to provide a reference for the treatment of acne scars in clinical practice.

Copyright © 2022 Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences, and Chinese Medical Association, published by Wolters Kluwer, Inc.
This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.
Acne scarring has a high incidence and is difficult to treat, which has a great impact on the physical and mental health of patients. Thus, the standardization of acne scar treatment is of great clinical significance. From the perspective of evidence-based medicine, experts from relevant societies have analyzed and summarized the evaluation and treatment strategies used for acne scars to standardize the treatment and provide a reference for clinicians at all levels to treat acne scars.
According to an American epidemiological survey, acne scars occur in about 43% of patients with acne, and patients with severe acne have a significantly higher risk of acne scars than those with mild and moderate acne.1 A Chinese survey showed that the prevalence of acne scars is about 7.1% in the general adolescent population, and that acne rarely appears before the age of 13 years.2 Different types of atrophic scars may appear on the same individual, while hypertrophic scars and keloids are more common in darker skinned individuals and occur mainly on the trunk and mandible.3
Factors affecting acne scar formation include the successful control of acne in the early stage, body mass index, sex, and family history of severe acne.4
Pathogenic microorganisms such as Propionibacterium acnes stimulate the activation and proliferation of CD4+ T cells and B cells, activate platelets and complement, release inflammatory factors, induce an increase in the expression of matrix metalloproteinases, disorder the degradation and synthesis of collagen fibers, and participate in the formation of acne scars. Inflammatory pathways such as nuclear factor kB, activator protein 1, and toll-like receptor activate the inflammatory cascade, promote local chemotaxis of inflammatory cells, destroy pilosebaceous units, aggravate local tissue damage, and promote scar formation.5
Some researchers believe that long-term maintenance of inflammatory papules is characterized by B-cell infiltration, and that the severity of acne scars is closely related to the severity and duration of acne and to changes in the structure of sebaceous glands. Inhibition of excessive inflammation and regulation of transforming growth factor b1 signaling in the early stage of acne promotes normal extracellular matrix metabolism and prevents the formation of acne scars.6
The formation process of acne scars is divided into the inflammatory exudation stage, repair stage, and scar stage. Hypertrophic acne scar formation is divided into the proliferative stage, setdown stage, and mature stage.7,8,9
Acne scars are mainly divided into atrophic and hypertrophic scars, with atrophic being the most common; keloids may also occur.7,10 According to the depth and size of damage, atrophic acne scars are further divided into icepick, boxcar, and rolling types. The icepick type is the most common, accounting for 60%-70% of acne scars. The icepick type presents as a deep V-shaped scar with a diameter of less than 2 mm that is deep to the dermis or even subcutis, with steep edges like an icepick, and its formation is associated with local collagen damage. Boxcar type scars account for about 20%-30% of acne scars, and are U-shaped with a diameter of about 1.5-4 mm, varying depth, and a wide base. Rolling type scars account for about 15%-25% of acne scars, and are W-shaped with the widest diameter of 5 mm, a shallow depth, and an undulating appearance. Hypertrophic scars and keloids are mainly distributed in the lower jaw and chest, shoulder and back, presenting as hard-textured nodules or plaques ranging in color from reddish to dark red.10
Acne scars are usually graded according to the appearance or degree of improvement after treatment. This method is simple and intuitive, but subjective. An example of this method is the "global scar quality score" of the qualitative global scarring grading system (GSS) (Table 1),11 which has been used in many clinical studies due to its specific and repeatable definition. The visual analog scale12 is based on an image scoring system and is a simple and reliable method of scoring blood supply, pigmentation, patient acceptability, observer comfort, and appearance. The Echelle d0 Evaluation Clinique des Cicatrices d0 acne (ECCA) (Table 2) assigns weighted scores to different types of scars to give a final total score in combination with the number of each type of scar.13 Similar to the ECCA is the quantitative GSS (Table 3).14 The ECCA and quantitative GSS scores are objective and are used to assess both atrophic and hypertrophic scars, and thus are used in many clinical studies; however, the relatively cumbersome calculation may limit their application. Hypertrophic scars and keloids are assessed using the Vancouver Scar Scale (Table 4)15 or the patient and observer scar assessment scale (Table 5),16 with the latter considering the patient's symptoms in the evaluation. Three-dimensional photography, skin ultrasonography, and a silicone inverted mold can be used to objectively measure scar volume, but require specific detection equipment and materials. At present, no single acne scar evaluation system is widely used, and the appropriate evaluation method is selected for clinical or scientific research.
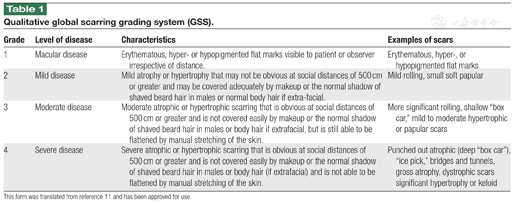
Qualitative global scarring grading system (GSS).
Qualitative global scarring grading system (GSS).
| Grade | Level of disease | Characteristics | Examples of scars |
|---|---|---|---|
| 1 | Macular disease | Erythematous, hyper- or hypopigmented flat marks visible to patient or observer irrespective of distance. | Erythematous, hyper-, or hypopigmented flat marks |
| 2 | Mild disease | Mild atrophy or hypertrophy that may not be obvious at social distances of 500 cm or greater and may be covered adequately by makeup or the normal shadow of shaved beard hair in males or normal body hair if extra-facial. | Mild rolling, small soft papular |
| 3 | Moderate disease | Moderate atrophic or hypertrophic scarring that is obvious at social distances of 500 cm or greater and is not covered easily by makeup or the normal shadow of shaved beard hair in males or body hair if extrafacial, but is still able to be flattened by manual stretching of the skin. | More significant rolling, shallow "box car," mild to moderate hypertrophic or papular scars |
| 4 | Severe disease | Severe atrophic or hypertrophic scarring that is obvious at social distances of 500 cm or greater and is not covered easily by makeup or the normal shadow of shaved beard hair in males or body hair (if extrafacial) and is not able to be flattened by manual stretching of the skin. | Punched out atrophic (deep "box car" ), "ice pick," bridges and tunnels, gross atrophy, dystrophic scars significant hypertrophy or keloid |
This form was translated from reference 11 and has been approved for use.
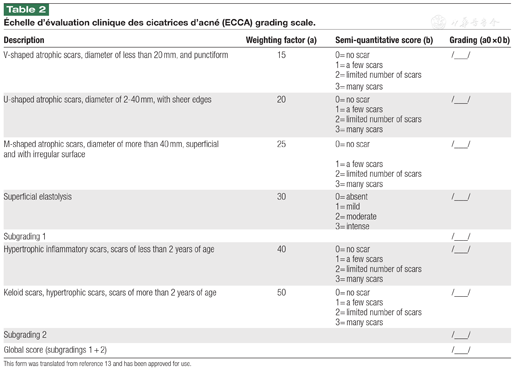
Échelle d'évaluation clinique des cicatrices d’acné (ECCA) grading scale.
Échelle d'évaluation clinique des cicatrices d’acné (ECCA) grading scale.
| Description | Weighting factor (a) | Semi-quantitative score (b) | Grading (a0 ×0 b) |
|---|---|---|---|
| V-shaped atrophic scars, diameter of less than 20 mm, and punctiform | 15 | 0= no scar | /___/ |
| 1= a few scars | |||
| 2= limited number of scars | |||
| 3= many scars | |||
| U-shaped atrophic scars, diameter of 2-40 mm, with sheer edges | 20 | 0= no scar | /___/ |
| 1= a few scars | |||
| 2= limited number of scars | |||
| 3= many scars | |||
| M-shaped atrophic scars, diameter of more than 40 mm, superficial and with irregular surface | 25 | 0= no scar | /___/ |
| 1= a few scars | |||
| 2= limited number of scars | |||
| 3= many scars | |||
| Superficial elastolysis | 30 | 0= absent | /___/ |
| 1= mild | |||
| 2= moderate | |||
| 3= intense | |||
| Subgrading 1 | /___/ | ||
| Hypertrophic inflammatory scars, scars of less than 2 years of age | 40 | 0= no scar | /___/ |
| 1= a few scars | |||
| 2= limited number of scars | |||
| 3= many scars | |||
| Keloid scars, hypertrophic scars, scars of more than 2 years of age | 50 | 0= no scar | /___/ |
| 1= a few scars | |||
| 2= limited number of scars | |||
| 3= many scars | |||
| Subgrading 2 | /___/ | ||
| Global score (subgradings 1 + 2) | /___/ |
This form was translated from reference 13 and has been approved for use.
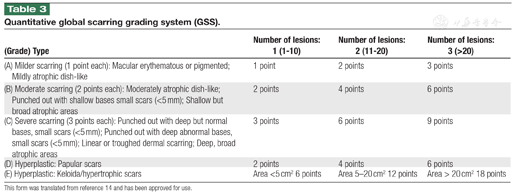
Quantitative global scarring grading system (GSS).
Quantitative global scarring grading system (GSS).
| (Grade) Type | Number of lesions: 1 (1-10) | Number of lesions: 2 (11-20) | Number of lesions: 3 (>20) |
|---|---|---|---|
| (A) Milder scarring (1 point each): Macular erythematous or pigmented; Mildly atrophic dish-like | 1 point | 2 points | 3 points |
| (B) Moderate scarring (2 points each): Moderately atrophic dish-like; Punched out with shallow bases small scars (<5 mm); Shallow but broad atrophic areas | 2 points | 4 points | 6 points |
| (C) Severe scarring (3 points each): Punched out with deep but normal bases, small scars (<5 mm); Punched out with deep abnormal bases, small scars (<5 mm); Linear or troughed dermal scarring; Deep, broad atrophic areas | 3 points | 6 points | 9 points |
| (D) Hyperplastic: Papular scars | 2 points | 4 points | 6 points |
| (E) Hyperplastic: Keloida/hypertrophic scars | Area <5 cm2 6 points | Area 5-20 cm2 12 points | Area > 20 cm2 18 points |
This form was translated from reference 14 and has been approved for use.
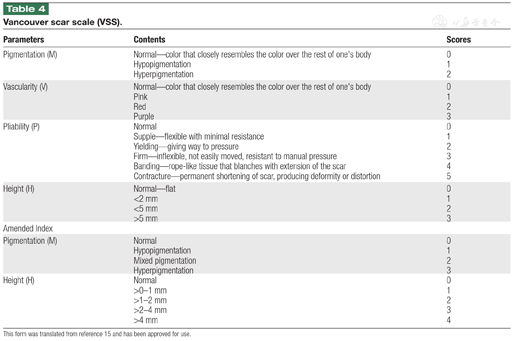
Vancouver scar scale (VSS).
Vancouver scar scale (VSS).
| Parameters | Contents | Scores |
|---|---|---|
| Pigmentation (M) | Normal—color that closely resembles the color over the rest of one's body | 0 |
| Hypopigmentation | 1 | |
| Hyperpigmentation | 2 | |
| Vascularity (V) | Normal—color that closely resembles the color over the rest of one's body | 0 |
| Pink | 1 | |
| Red | 2 | |
| Purple | 3 | |
| Pliability (P) | Normal | 0 |
| Supple—flexible with minimal resistance | 1 | |
| Yielding—giving way to pressure | 2 | |
| Firm—inflexible, not easily moved, resistant to manual pressure | 3 | |
| Banding—rope-like tissue that blanches with extension of the scar | 4 | |
| Contracture—permanent shortening of scar, producing deformity or distortion | 5 | |
| Height (H) | Normal—flat | 0 |
| <2 mm | 1 | |
| <5 mm | 2 | |
| >5 mm | 3 | |
| Amended Index | ||
| Pigmentation (M) | Normal | 0 |
| Hypopigmentation | 1 | |
| Mixed pigmentation | 2 | |
| Hyperpigmentation | 3 | |
| Height (H) | Normal | 0 |
| >0-1 mm | 1 | |
| >1-2 mm | 2 | |
| >2-4 mm | 3 | |
| >4 mm | 4 | |
This form was translated from reference 15 and has been approved for use.
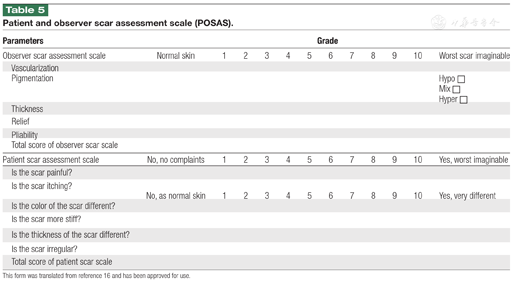
Patient and observer scar assessment scale (POSAS).
Patient and observer scar assessment scale (POSAS).
| Parameters | Grade | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observer scar assessment scale | Normal skin | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Worst scar imaginable | |
| Vascularization | |||||||||||||
| Pigmentation | Hypo □ | ||||||||||||
| Mix □ | |||||||||||||
| Hyper □ | |||||||||||||
| Thickness | |||||||||||||
| Relief | |||||||||||||
| Pliability | |||||||||||||
| Total score of observer scar scale | |||||||||||||
| Patient scar assessment scale | No, no complaints | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Yes, worst imaginable | |
| Is the scar painful? | |||||||||||||
| Is the scar itching? | No, as normal skin | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Yes, very different | |
| Is the color of the scar different? | |||||||||||||
| Is the scar more stiff? | |||||||||||||
| Is the thickness of the scar different? | |||||||||||||
| Is the scar irregular? | |||||||||||||
| Total score of patient scar scale | |||||||||||||
This form was translated from reference 16 and has been approved for use.
It is necessary to educate patients about the causes of acne formation, processes, and outcomes, and to use scientifically proven methods for the prevention and cure of acne scars until their acne repair has stabilized for more than 6 months.
Age: Acne remains the greatest risk factor for scarring in youth, and reduces with age.
Sex: Acne scars affect more males than females.
Family history: Patients with a family history of scars have an increased risk of acne scars.
Acne phase: The risk of scarring is reduced when acne is cured in the red papular phase, and there is a greater risk of acne scarring when the skin is visibly damaged.
Affected body part: Acne scars are more common on the face, jaw, chest, shoulder, and back.
Treatment: Early standardized and appropriate treatments can avoid or reduce the occurrence of acne scars.
Acne scar formation is effectively reduced by active treatment of moderate to severe acne and by early intervention and cure. The following precautions may help reduce acne scarring: (a) a healthy diet with balanced nutrition and limited amounts of sugar and greasy food; (b) living in an orderly manner, and avoiding staying up late and sun exposure; (c) moderate exercise and maintenance of a normal weight; (d) reduction of anxiety and depression; (e) performing appropriate daily skin care to keep the skin clean, but not cleaning excessively; (f) avoidance of squeezing and scratching lesions to prevent breaking the skin.
In the early stage of acne scar formation, anti-inflammatory medications are recommended to prevent further skin necrosis and obvious scar formation. Recommended active interventions in the early stage include intense pulsed light and a 560 nm or 590 nm filter or 500-600 nm mixed spectral line intense pulsed light with a low-energy mode for continuous daily treatment until the improvement or subsidence of inflammatory erythematosus. At the mature stage of acne scar formation, the recommended interventions include exfoliative lattice lasers such as CO2 and neodymium-dopped yttrium aluminium garnet (Er:YAG) lattice lasers, fractional microneedle radiofrequency, or traditional Chinese plum needle rolling needle for the treatment of atrophic scars. Mild atrophic scars can also be treated with plasma therapy or exfoliative lattice laser therapy. Hypertrophic scars should be treated with drugs combined with photoelectric therapy, such as the injection of a long-acting glucocorticoid combined with laser stripping. For patients with keloid scar formation, the recommended treatments are drug therapy, photoelectric combined with radiotherapy, or surgery combined with radiotherapy.
Silicone improves the scar epidermal structure and prevents scar hyperplasia and contracture and is mostly used for the prevention and treatment of hypertrophic acne scars. The recommended duration of use is more than 6 months.
Heparin sodium allantoin inhibits fibroblast proliferation to make the scar surface more elastic and is used for the treatment of hypertrophic and keloid scars. The recommended duration of use is more than 6 months.
Glucocorticoids reduce inflammation, inhibit fibroblast proliferation, induce apoptosis, and reduce collagen synthesis, but may cause adverse reactions including skin atrophy, telangiectasia, and hypopigmentation. Directions for usage: 1.0 mL of compound betamethasone (7 g/L) or triamcinolone acetonide solution (10 g/L) + 1.0 mL of lidocaine solution (20 g/L) applied once a month.
Botulinum toxin A inhibits the release of acetylcholine from nerve endings, relaxes muscle fibers, reduces local tension, and reduces keloid formation. Possible adverse reactions include dysfunction caused by local muscle paralysis and subcutaneous congestion at the injection site. Directions for usage: 20-50 U/mL is usually prepared for injection into keloid dermis, and the total dose should be less than 100 U per monthly injection according to the volume of scarring.
Fluorouracil inhibits thymidylate synthase, affects fibroblast proliferation, blocks transforming growth factor b-mediated expression of the type I collagen gene, and reduces collagen production. Fluorouracil is often used in combination with triamcinolone acetonide, and patients must undergo routine blood testing during use. Fluorouracil cannot be used by pregnant or lactating women. Directions for usage: triamcinolone acetonide (10 g/L) and 2.5% fluorouracil injection are extracted to prepare a mixed solution in a ratio of 3:1-1:1. The maximum single dose is 2 mL triamcinolone acetonide and 0.5 mL fluorouracil. Patients with excessive skin lesions should be injected once every 10-14 days. If the needle wound is not healed or the drug is not completely absorbed, the interval between injections can be extended to 15-30 days.
Bleomycin is a cytotoxic drug that improves the appearance of pathological tissues and significantly relieves the itching and pain caused by keloids. Directions for usage: 1.5 IU/mL bleomycin solution is injected every 0.5 cm and repeated once or twice a month according to the patient's needs.
Oral drugs such as asiaticosides, retinoids, and tranilast can be administered to inhibit the proliferation of fibroblasts and reduce the production of collagen fibers to prevent scar formation in the early stage. However, these drugs are rarely used in clinical practice.
Laser therapy is based on the principles of selective photothermal action and focal photothermal action. The types of lasers include lattice laser, long pulsewidth Nd: YAG laser, and pulsed dye laser.
Atrophic scars: Exfoliative lattice lasers (lattice Er:YAG and lattice CO2) form a microcolumnar gasification zone and hot solidification necrotic zone in tissue, promoting epidermal regeneration and collagen remodeling. Treatment parameters need to be individually set according to the type and location of acne scars.17 Exfoliative lattice lasers are used to treat shallow boxcar type and rolling type atrophic scars. Non-exfoliative lattice lasers include lattice Er:Glass lasers, thulium fiber lasers, and focused lattice lasers. Compared with exfoliative lattice lasers, non-exfoliative laser therapy requires a shorter recovery period, but has a weaker collagen remodeling ability, and often needs more treatment sessions to achieve similar efficacy. Long pulsewidth Nd:YAG laser therapy can also be used to treat atrophic scars. Hypertrophic scars/keloids: Pulsed dye laser therapy and long pulsewidth Nd:YAG laser therapy reduce microvessels and promote collagen degradation and remodeling, thereby improving scar erythema, thickness, and flexibility, which is useful in treating erythematous hypertrophic scars and keloids. Exfoliative laser therapy can be used to vaporize stable hypertrophic scars on areas such as the nose. Exfoliative lattice laser therapy releases scar adhesions and improve scar elasticity. For severe keloids, it is recommended to combine laser therapy with local glucocorticoid injection, superficial X-ray radiation, surgical resection, and other treatments.
Intense pulsed light acts on hemoglobin and collagen and is used to improve shallow atrophic scars and early erythematous hypertrophic scars. Intense pulsed light therapy can be combined with drug injection or laser treatment.
Radiofrequency therapy can be used in combination with laser therapy and/or for patients with atrophic acne scars with inflammatory acne lesions. Radiofrequency therapy does not aggravate the original active acne lesions and can reduce the sebum level and sebum overflow rate, which is useful in patients with inflammatory acne. The main adverse reactions include pain, transient erythema, and edema, while pigmentation is rare.
Plasma therapy mainly uses the energy released by plasma to produce heat and exfoliation to improve scarring, and is suitable for treating shallow atrophic scars. The recommended treatment methods include multiple, single round, low energy density or single, single round, high energy density; the former may have a shorter recovery time.18
Photodynamic therapy is limited to patients with moderate and severe acne caused by Propionibacterium acnes; however, there is still a lack of evidence regarding the use of photodynamic therapy for acne scars.
Skin grinding is suitable for rolling type and shallow boxcar type scars (evidence level I, recommended strength++), but has poor efficacy for icepick type and deep boxcar type scars.10 This technique enables the precise and controlled removal of scar edges without thermal damage, and the effectiveness of treatment is highly dependent on the skill and experience of the operator. A wide range of grinding requires general anesthesia, takes up to 2 weeks to heal, and is accompanied by long-term postoperative erythema, which may cause pigmentation and scar hyperplasia.
Subcutaneous separation is mainly suitable for rolling type scars (Level of Evidence III, recommended strength+++), and is partially effective for icepick type and boxcar type scars. The operation is simple and can be completed under local anesthesia, and can be combined with filling and laser technology. Multiple treatments may be required to obtain satisfactory results. Adverse reactions include temporary petechiae, swelling, bleeding, paresthesia, and inflammatory papules. Subcutaneous separation can be divided into sharp needle separation and blunt needle separation.19
A trephine with an inner diameter of 0.8-2.5 mm is often used clinically. Trephine tissue extraction is suitable for treating hypertrophic acne scars and keloids, while trephine tissue promotion is suitable for icepick type and boxcar type acne scars with clear edges and a normal basal appearance. Trephine tissue transplantation is suitable for treating hyperpigmentation and deep icepick type acne scars.4
Surgical resection is suitable for large scars on the mandibular angle, keloids caused by acne on the upper torso, and deep atrophic scars that cover a large area. Surgical methods include simple resection and suture, Z or W plasty, cicatrectomy, skin grafting, flap transfer, and skin dilation.20 Superficial X-ray therapy is required after keloid surgery.
Filling therapy fills the skin lesions by injection or surgery and stimulates fibroblasts to produce collagen fibers and fibrous tissues to replenish the volume and smooth scars. Filling therapy is mostly used for large and deep atrophic scars, especially boxcar type and rolling type scars (Level of Evidence V, recommended strength ++). The most common fillers are autologous fat, fat glue, autologous cells, hyaluronic acid, and poly-L-lactic acid.21
Autologous fat grafting (AFG) supplements the missing tissue, promotes the formation of new blood vessels, and improves skin elasticity to improve the appearance of scars. AFG has the advantages of easy access and no rejection or allergies, but the fat survival rate is unstable and multiple treatments are often required to achieve satisfactory results. Stromal vascular fraction gel (SVF-GEL) is a gel-like extract obtained by mechanically cutting autologous fat and removing lipid droplets by centrifugation. The main components of SVF-GEL are extracellular matrix, adipose stem cells, and vascular endothelial cells.22 Compared with simple AFG, SVF-GEL injection results in less inflammation, less swelling, a higher survival rate, and a relatively stable effect. Comparative studies have shown that SVF-GEL is more effective than CO2 fractional laser therapy in the treatment of acne scars. The severity of scars, percentage of scarred area, transdermal water loss, and skin water content are all significantly improved for 3 months after one SVF-GEL treatment, and the therapeutic effect of one SVF-GEL treatment is equivalent to that of three fractional laser treatments.23
In autologous fibroblast transplantation, skin is removed from a non-exposed part of the patient. The fibroblasts from this skin are isolated and cultivated for several weeks and then injected into the scar to form new collagen to help reshape the extracellular matrix. Autologous fibroblast transplantation has the advantages of permanent filling and low immunogenicity.
Another commonly used tissue filler is low cross-linked hyaluronic acid, which has the advantages of low immunogenicity and absorbability.
Superficial chemical peeling is used to treat shallow atrophic acne scars and scars with postinflammatory hyperpigmentation (PIH). Glycol acid peeling promotes epidermal renewal and thickening, while also promoting the proliferation of acid mucopolysaccharides, collagen fibers, and elastic fibers in the papillary layer of the dermis. A mixture of 20%-70% glycolic acid, 92% lactic acid, and 25%-30% salicylic acid improves skin texture, reduces PIH, prevents scarring in the early stage, and flattens and shrinks the surface of shallow atrophic scars during the adjuvant treatment of acne lesions.24 Jessner solution (14 g of resorcinol, 14 g of salicylic acid, 14 g of 85% lactic acid, and ethanol to make up 100 mL) treats acne and has a certain effect on superficial scars, and is often used in combination with other exfoliation methods to increase the depth of chemical peeling.25 A compound acid composed of 10% mandelic acid and 20% salicylic acid is as effective as 35% glycolic acid, but the former is milder and has a lower risk of PIH.26 Superficial chemical peeling is recommended to treat atrophic icepick type acne scars.
Although the use of trichloroacetic acid or phenol for middle or deep exfoliation is more effective in the treatment of atrophic deep boxcar type acne scars, deep exfoliation is only recommended with caution in the Chinese population because dark-skinned people are prone to PIH.
Traditional Chinese medicine therapy is divided into internal and external treatments. Internal treatment is based on syndrome differentiation. For example, the treatment of blood stasis and toxin accumulation is used to promote blood circulation to remove blood stasis, detoxify, and dispel stagnation. External treatments are prepared with Chinese herbal medicines as external washing prescriptions, tinctures, and ointments. The main aim of external treatment is to promote blood circulation, remove blood stasis, soften the hard texture, and dispel knots. For atrophic scars, plum blossom needles, rolling needles, small needle knives, fire needles, moxibustion, and other methods are used to clear the meridians and regulate Qi and blood. For hypertrophic scars, asiaticoside ointment, black cloth ointment,27 and other drugs are used externally. Dark-colored scars are treated with local bloodletting, acupuncture, or fire needles to dispel blood stasis, regenerate new tissue, and treat soft and hard knots; if there is a lot of tension, a small needle knife is used to loosen it.
Biotherapy involves treatment with biological macromolecules and is divided into cell therapy and non-cell therapy (such as autologous fibroblast therapy) for depressed acne scars. However, the clinical effect needs further evaluation.
ReCell technology is also called skin active cell transplantation and is mainly used in conjunction with skin abrasion (Level of Evidence V, recommended strength +). The wound healing time is shorter after ReCell therapy than after skin abrasion alone, and the outer dressing can be removed only 5 days after ReCell surgery. ReCell therapy also has a low incidence of postoperative pigmentation and scar hyperplasia, which is most advantageous in the treatment of rolling type and shallow boxcar type scars.28
Intradermal injection or topical application of platelet-rich plasma is mainly used as an auxiliary technology combined with microneedle therapy and exfoliative lattice laser therapy to improve the effectiveness of scar treatment. Platelet-rich plasma therapy is simple and safe with no reported adverse reactions, but lacks a standardized treatment plan.29
There is currently a lack of high-quality research evaluating the effectiveness and safety of stem cell therapy. Injecting autologous bone marrow mesenchymal stem cells into scars may improve the appearance of atrophic scars,30 and is expected to be a future research direction.
Microneedle therapy causes mechanical damage, induces inflammation, causes platelet aggregation, chemoattracts neutrophils, and macrophages, and releases transforming growth factors a and b and platelet-derived growth factors to promote collagen synthesis of fibers and elastic fibers. In addition, the micropores created by the microneedles facilitate drug absorption and promote wound healing.31 Although microneedle therapy can cause postoperative erythema and dry skin, these adverse effects are well tolerated by most patients. Microneedle therapy alone is relatively effective in the treatment of atrophic acne scars, and achieves a greater effect when combined with other therapies, such as platelet-rich plasma, chemical ablation, injection filling, or laser. For acne scars with an uneven surface, the injection of triamcinolone acetonide and compound betamethasone into fibrotic lesions helps soften hypertrophic scars.
The development of acne scars is effectively reduced by the early treatment of acne, control of excessive sebum secretion, and reduction of inflammatory response damage. However, once acne scars occur, the treatment is more challenging. Studies have shown that acne scars are significantly reduced by topical preparations that produce nitric oxide32 and long-term use of 0.3% adapalene/2.5% benzoyl peroxide compound preparations.33 The directions of future research include the continuous development and joint application of new treatment strategies, such as skin barrier function repair, maintenance of normal skin micro-ecology,34 application of stem cell technology, non-invasive collagen stimulation, and scar remodeling.
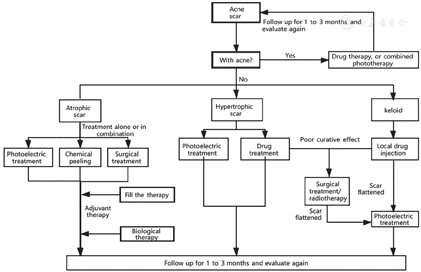
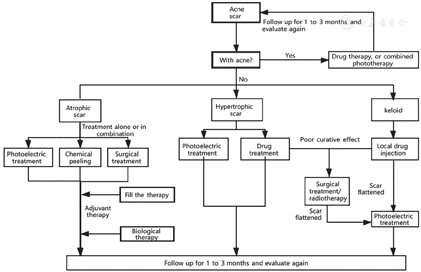
Figure 1 and Table 6 summarize the clinical pathway and evidence-based grade of acne scar treatments formulated by the Editorial Board of this Consensus.
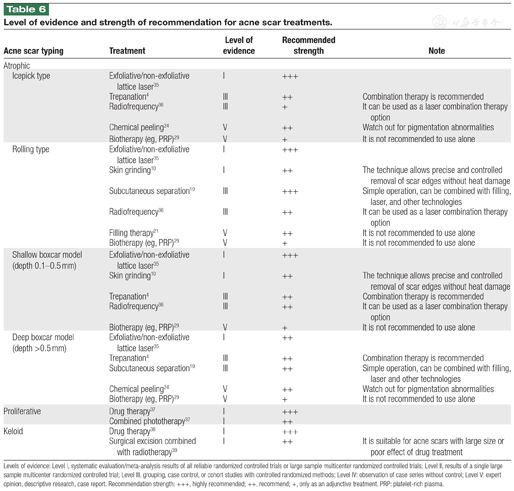
Level of evidence and strength of recommendation for acne scar treatments.
Level of evidence and strength of recommendation for acne scar treatments.
| Acne scar typing | Treatment | Level of evidence | Recommended strength | Note | |
|---|---|---|---|---|---|
| Atrophic | |||||
| Icepick type | Exfoliative/non-exfoliative lattice laser35 | I | +++ | ||
| Trepanation4 | III | ++ | Combination therapy is recommended | ||
| Radiofrequency36 | III | + | It can be used as a laser combination therapy option | ||
| Chemical peeling24 | V | ++ | Watch out for pigmentation abnormalities | ||
| Biotherapy (eg, PRP)29 | V | + | It is not recommended to use alone | ||
| Rolling type | Exfoliative/non-exfoliative lattice laser35 | I | +++ | ||
| Skin grinding10 | I | ++ | The technique allows precise and controlled removal of scar edges without heat damage | ||
| Subcutaneous separation19 | III | +++ | Simple operation, can be combined with filling, laser, and other technologies | ||
| Radiofrequency36 | III | ++ | It can be used as a laser combination therapy option | ||
| Filling therapy21 | V | ++ | It is not recommended to use alone | ||
| Biotherapy (eg, PRP)29 | V | + | It is not recommended to use alone | ||
| Shallow boxcar model (depth 0.1-0.5 mm) | Exfoliative/non-exfoliative lattice laser35 | I | +++ | ||
| Skin grinding10 | I | ++ | The technique allows precise and controlled removal of scar edges without heat damage | ||
| Trepanation4 | III | ++ | Combination therapy is recommended | ||
| Radiofrequency36 | III | ++ | It can be used as a laser combination therapy option | ||
| Biotherapy (eg, PRP)29 | V | + | It is not recommended to use alone | ||
| Deep boxcar model (depth >0.5 mm) | Exfoliative/non-exfoliative lattice laser35 | I | ++ | ||
| Trepanation4 | III | ++ | Combination therapy is recommended | ||
| Subcutaneous separation19 | III | ++ | Simple operation, can be combined with filling, laser and other technologies | ||
| Chemical peeling24 | V | ++ | Watch out for pigmentation abnormalities | ||
| Biotherapy (eg, PRP)29 | V | + | It is not recommended to use alone | ||
| Proliferative | Drug therapy37 | I | +++ | ||
| Combined phototherapy37 | I | ++ | |||
| Keloid | Drug therapy38 | I | +++ | ||
| Surgical excision combined with radiotherapy39 | I | ++ | It is suitable for acne scars with large size or poor effect of drug treatment | ||
Levels of evidence: Level I, systematic evaluation/meta-analysis results of all reliable randomized controlled trials or large sample multicenter randomized controlled trials; Level II, results of a single large sample multicenter randomized controlled trial; Level III, grouping, case control, or cohort studies with controlled randomized methods; Level IV: observation of case series without control; Level V: expert opinion, descriptive research, case report. Recommendation strength: +++, highly recommended; ++, recommend; +, only as an adjunctive treatment. PRP: platelet-rich plasma.
Doctors should inform the patients about realistic expectations, recovery time, treatment cost, and the importance of maintenance therapy before treatment. The types and depth of the scars and patient's skin type must be evaluated to enable the selection of the optimal therapeutic schedule and equipment. The affected area should be cleaned with a mild facial cleanser before treatment. A healthy diet is recommended before and after treatment. Pretreatment, immediately posttreatment, and follow-up photographs should be taken; the position, background, angle, direction, distance, and lighting should be optimized.
The appropriate treatment mode and parameters should be chosen based on the patient's skin type and the type and depth of the scars. Clinicians must observe the immediate treatment response, including the degree of redness, oozing, eschar formation, and penetration depth. Different photoelectric therapies result in different skin reactions. Non-exfoliative phototherapy results in only slight redness and swelling, while exfoliative laser therapy causes immediate spot-like whitening.
Clinicians must monitor the postoperative reaction, including the degree of skin swelling, peeling, and oozing, and observe the recovery to identify infection, scab formation, and erythema. Aseptic epidermal growth factor, collagen spray or gel, or a medical hyaluronic acid or collagen mask should be used as appropriate to promote repair. After exfoliative laser treatment, patients must avoid contacting water as much as possible before epidermal healing; when necessary, a sterile physiological sodium chloride solution can be used for cleaning. The posttreatment scab should be left to drop off naturally. It is particularly important to prevent infection after exfoliative photoelectric treatment. Mupiroxacin, erythromycin ointment (or eye ointment), and other antibiotics can be used to prevent infection, when necessary. It is important to moisturize the skin after non-exfoliative phototherapy and after exfoliative phototherapy once the scab has fallen off. Sun protection is essential. Patients should wear a sunscreen shirt or shelter under an umbrella and wear a mask, but should use sun cream with caution to prevent allergic reactions.
Patients are instructed to abstain from alcohol and smoking and are evaluated for heart and lung diseases, history of previous surgery, and medication allergies. The skin in the surgical area is prepared and evaluated to determine the type, size, range, color, depression or bulge, and texture of the scar. Pre-, intra-, and postoperative photographs should be taken under good conditions.
When performing skin grinding, clinicians must prevent the grinding depth from exceeding the superficial dermis to the deep dermis and monitor the amount of intraoperative bleeding and oozing. If the acne scar is removed surgically, clinicians must avoid overly deep excision, ensure that blood vessels and nerves are avoided, and completely stop the bleeding. The excision scope should not be too large but should be limited within the skin lesion boundary as far as possible to avoid excessive suture tension and later scar enlargement.
Postoperative monitoring is important to detect any adverse reactions such as oozing, exudation, redness, and swelling at the suture line. Regular dressing changes are required to prevent wound infection. After the wound has healed, patients must moisturize and apply sunscreen; anti-scar drugs can be administered to prevent scar hyperplasia.
Prior to chemical peeling, a thorough consultation and examination should be conducted to determine the skin type, degree of photoaging and sebum activity, and detect PIH, hypertrophic scarring, and local bacterial or viral infection.40 During the operation, clinicians must use the appropriate stripping agent concentration and stripping time and observe the skin reaction. Patients should use a mild moisturizing agent for 1 week postoperatively, wait for the scab to fall off naturally without force, apply sunscreen, and consume a healthy diet.
Doctors should inquire about the patient's medical history, accurately grade the acne scar using the Vancouver Scar Scale, visual analog scale, or POSAS, and inform the patient about potential adverse reactions to reduce the psychological burden on patients when adverse reactions occur.
During treatment, the condition of the treated area should be dynamically observed and recorded, including the presence of any adverse reactions such as redness, swelling, burning, and pain. In addition, the patient's general condition and possible adverse reactions (such as allergy and embolism) should be noted.
The wound will ooze after the injection of biologics and must be kept dry and clean with medical wound dressings. Patients who have undergone ReCell therapy and biotherapy combined with laser or microneedle therapy must be vigilant about sun protection. Moreover, patients who have undergone ReCell therapy should be given anti-infection treatment to prevent local infection.
In recent years, new methods and technologies for the treatment of acne scars have continuously emerged in China and abroad. This consensus is based on evidence-based medicine and aims to provide a convenient reference for clinicians at all levels to treat acne scars. The current clinical evidence for the treatment of acne scars is mostly of low quality. Future multicenter, standardized clinical trials with large sample sizes are warranted to provide high-quality clinical evidence for the development of evidencebased guidelines for the diagnosis and treatment of acne scars.
The Guideline in Chinese was published on Chinese Journal of Dermatology. 2021, 54(9):747-756. doi:10.35541/cjd.20210182.
The authors reported no conflicts of interest.






























